Evidence of activation of the protein C pathway during acute... damage induced by Mediterranean spotted fever
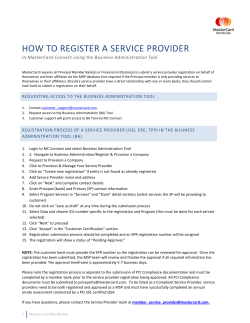
From www.bloodjournal.org by guest on October 28, 2014. For personal use only. 1991 78: 416-422 Evidence of activation of the protein C pathway during acute vascular damage induced by Mediterranean spotted fever V Vicente, F Espana, D Tabernero, A Estelles, J Aznar, S Hendl and JH Griffin Updated information and services can be found at: http://www.bloodjournal.org/content/78/2/416.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved. From www.bloodjournal.org by guest on October 28, 2014. For personal use only. Evidence of Activation of the Protein C Pathway During Acute Vascular Damage Induced by Mediterranean Spotted Fever By Vicente Vicente, Francisco Espatia, Dolores Tabernero, Amparo Estelles, Justo Aznar, Sylvia Hendl, and John H. Griffin Mediterranean spotted fever (MSF) is a rickettsiosis that induces widespread microvascular injury. To obtain quantitative information on the in vivo activation and inactivation of the protein C system during the acute phase of endothelial damage, several components of the protein C pathway were studied in 28 MSF patients. Upon admission (day l), patients showed clear evidence of endothelial damage as reflected by the significant decrease in the ratio VIII:C/vWF:Ag (0.36f 0.14,mean SD) compared with normals (0.98f 0.14),and clinical and laboratory signs of hemostatic alterations such as decreased platelet count, positive fibrinogedfibrin degradation products, and increased thr0mbin:antithrombin-Ill complex levels. Antigenic protein C (72% -C 18%) and protein C inhibitor (PCI) (41% % 20%) were significantly decreased (P < ,001).Complexes of activated protein C (APC) with PCI or with %-antitrypsin (a,AT) and of plasma kallikrein with PCI (KK:PCI) were measured using sandwich enzyme-linked immunosorbent assays. APC:qAT complex levels were increased in patients at day 1 (27 k 13 ng/mL) compared with controls (72 2 ng/mL), and APC:PCI and KK:PCI complexes, which were not detectable in any of the controls, were present in 57% and 75% of the 28 MSF patients, with mean levels of 1 1 k 5 and 46 ? 16 ng/mL, respectively. After remission of the disease (day 30). a trend toward normal values in the majority of the parameters studied was found. This study shows that, in the course of endothelial injury, MSF patients experience a generalized activation of the protein C pathway, resulting in consumption of protein C and PCI, and in the appearance of APC:inhibitor complexes. Moreover, these data provide the evidence that KK:PCI circulating complexes occur in vivo. o 1991by The American Society of Hematology. M which these cells participate is the protein C anticoagulant pathway. The cell surface possesses a thrombin-binding protein, thrombomodulin (TM). Thrombin bound to TM initiates protein C activation on endothelial surfaces.6 Activated protein C (APC) then catalyzes the proteolytic inactivation of factors Va and VIIIa with its cofactor protein S. APC has also been reported to have profibrinolytic activity, possibly by neutralizing plasminogen activator inhibitors.’.’ In vivo studies have shown that APC is antithrombotic in a baboon model of platelet-dependent thrombosis8and in a dog model of venous thrombosis.’ APC is inhibited by a heparin-dependent plasma inhibitor named protein C inhibitor (PCI),’” which has been purified and chara~terized’.’’.’~ and the sequence of its cDNA reported.13Plasma contains another major inhibitor of APC that is heparin-inde~endent,’~ which has been shown to be a,-antitrypsin (a,AT).I5 We demonstrated that APC forms complexes in vivo with each of these inhibitors in several clinical situations where activation of coagulation has oc~urred,’~.’’ and have suggested that the measurement of APC complexes may provide sensitive parameters for specific detection of activation of the clotting and protein C pathways. As indicated, any injury of the endothelial cells that affects the appropriate expression of the protein C system could potentially lead to a hypercoagulable state and result in thrombotic complications. The acute phase of MSF fulfills the criteria of endothelial cell perturbation that may lead to such a state. This study was undertaken to obtain qualitative and quantitative information on the activation and inactivation of protein C in MSF and its distribution between its known inhibitors, PCI and a,AT, during the acute and subacute phases of this vascular infectious disease. * EDITERRANEAN spotted fever (MSF) is a rickettsiosis belonging to the spotted fever group of infections and is caused by tick-borne Rickettsia conorii. MSF shares with other rickettsiosis one dominant feature, widespread microvascular injury.’ Rickettsiae infect human endothelial cells, proliferate intracellularly by binary fission, and spread contiguously to infect numerous adjacent endothelial cells.’ Rickettsial vasculitis, in fact, comprises endothelial injury (swelling and necrosis) and the immune and phagocytic host responses (lymphocytes and macrop h a g e ~ ) .The ~ pathophysiologic effects of vascular injury include increased vascular permeability, edema, hypovolemia, and activation of humoral inflammatory and coagulation mechanisms.4 As discussed previously: endothelial damage could be the principal mechanism responsible for triggering the hypercoagulation state that occurs in the acute phase of MSF. Intact vascular endothelium provides several anticoagulant mechanisms for the maintenance of blood fluidity and the prevention of thrombosis. One of the several systems in From the Department of Medicine, School of Medicine, Murcia, and Research Center and Department of Clinical Pathology, Hospital “La Fe, ” Valencia, Spain; and Committee on Vascular Biology and Department of Molecular and Experimental Medicine, Research Institute of Scripps Clinic, La Jolla, CA. Submitted December 24,1990; accepted March 19, 1991. Supported by research grants from Fondo de Investigaciones Sanitarias de la Seguridad Social (9010586) and from CICYT (No. PA 85-0347), Spain, and from the National Institutes of Health (HL31950). Address reprint requests to Francisco Esparia, PhD, Hospital “La Fe, ” Centro de Investigacibn, Av. Campanar, 21, 46009 Valencia, Spain. The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact. 0 1991 by The American Socieiy of Hematology. 0006-4971191l7802-0OI7$3.00/0 416 MATERIALS AND METHODS Patient data. Twenty-eight consecutively admitted patients (age range 5 to 86 years, mean 59) from the 1988-1989 epidemic in Salamanca (Spain) and 30 normal subjects (age range 18 to 65 years, mean 39) were examined. Diagnosis of MSF was confirmed Blood, Vol 78, No 2 (July 15). 1991: pp416-422 From www.bloodjournal.org by guest on October 28, 2014. For personal use only. 417 PROTEIN C ACTIVATION IN SPOlTED FEVER by clinical findings and by serologically measuring titters of antibody specific for this illness using indirect immunofluorescence? Blood samples were obtained on admission, ie, during the acute phase of the disease (day 1) and 30 days after the start of treatment (day 30). The elapsed time from the onset of symptoms (fever) to diagnosis ranged between 3 and 12 days (mean, 7 days). In the acute phase of the disease, two patients presented clinical signs and evident symptoms of deep vein thrombosis in their legs. The diagnosis was confirmed by ascending venography. However, all patients recovered favorably and did not exhibit any other clinical complications. Informed consent was obtained from all patients and control subjects before blood collection. Blood samples. Blood collection was made by venipuncture with a 19-gauge needle. Nine parts of blood were added to plastic tubes containing one part of 0.13 mol/L trisodium citrate with or without 50 mmol/L benzamidine. Blood samples were rapidly centrifuged at 2,50Cg for 20 minutes. The plasma was used fresh or snap-frozen in small portions and stored at -70°C until the assays were performed in series (less than 6 months). Pooled normal human plasma was made from 24 healthy donors and used as a reference. Blood samples for determination of protein C antigen, total and free protein S, PCI antigen, antithrombin I11 (AT-HI), a,AT, C4b-binding protein, and enzyme:inhibitor complexes were collected in citrate containing 50 mmol/L benzamidine. Protein S functional activity and protein C amidolytic activity were determined in samples collected with citrate alone. Quantitative assay of the protein C system components. Protein C antigen and amidolytic activity,’*anticoagulant protein S,I9 and PCI antigen and activitp were assayed as indicated before. Total and free protein S antigen were assayed by enzyme-linked immunosorbent assays (ELlSAs), as indicated by Deutz-Terlouw et a1,” using Complexes of APC specific anti-protein S polyclonal antib~dies.’~.’’ with PCI (APCPCI)20or with a,AT (APC:a,AT),” and complexes of plasma kallikrein (KK) with PCI (KK:PCI)’ were determined by using sandwich ELISAs, as reported. Briefly, microplates were coated with monoclonal antibody (MoAb) to protein C (for APC:PCI and APCa,AT complexes) or to PCI (for KK:PCl complexes), and complexes were detected with peroxidase-labeled polyclonal antibodies to either PCI or a,AT or KK, respectively. Reference curves were constructed with known amounts of in vitro preformed complexes. The detection limit of the assays in plasma was 1,3, and 15 ng/mL, respectively. Determination of other blood coagulation components. Platelets were counted with an electronic hematology analyzer (Hemalog-8; Technicon, Tarritown, NY). Factor VI11 procoagulant activity (V1II:C) was assayed in a one-stage test using platelet-poor plasma (PPP) from a patient with severe hemophilia A as substrate, as previously reported? Quantitative immunologic determinations of von Willebrand factor antigen (vWF:Ag), AT-111, a,AT, and C4bbinding protein were performed by a electroimmunoassay techniquex using rabbit antisera to these proteins (Behringwerke, Marburg, Germany). Factors 11, VII, IX, X, XI, and XI1 were assayed in one-stage tests using PPP obtained from patients congenitally deficient in the respective factors as substrate (Behringwerke), as previously reported? Fibrinogen was assayed by the Clauss methodz5and fibrin degradation products (FDP) by agglutination of particles coated with specific antibodies (Diagnostica Stago, Asnieres, France). Complexes of thrombin with AT-I11 (T:AT-111) were assayed by a sandwich ELISA (Enzygnost-TAT, Behringwerke AG) that uses a polyclonal antibody specific for neoantigenic determinants on thrombin as the capture antibody and peroxidase-labeled polyclonal antibody to AT-I11 as the tag. Statistical analysis. A normal (Gaussian) distribution of levels of each parameter in each group was checked using the KolmogorovSmirnov test. Variations in parameter levels in patient groups compared with levels in the normal control group were investigated using the Student’s t-test with two-tailedPfor significance. Comparisons between patients upon admission (day 1) and 30 days later were calculated with the Student’s t-paired test. All assay variables are represented by their mean and standard deviation. RESULTS Coagulationparameters. Table 1 shows the mean values of several blood coagulation parameters studied in 30 healthy subjects and in 28 MSF patients. Compared with the control group, MSF patients in the acute phase of disease (day 1) showed a significant decrease in platelet count and VIII:C/vWF:Ag ratio (P < .001) and a significant increase in vWF:Ag and fibrinogen (P < .OOl). At the time of diagnosis (day l), nine patients were detected as FDP positive ( > 10 pglmL). After 30 days of treatment (day 30), a significant increase in platelet number was observed when compared with the values at day 1 (P < .OOl). VIII:C/vWF:Ag ratio increased significantly (P < .001) at day 30 when compared with that at day 1, but it remained decreased compared with normal values (P < .Ol). vWFAg decreased during the course of the disease, but it remained increased compared with normal values (P < .001). Coagulation factors 11,VII, IX, X, XI, XII, and prekallikrein were in the normal range both before and after treatment. Table 2 shows the mean values of several components of the protein C pathway and other related parameters studied in normal subjects and in MSF patients. Compared with the control group, MSF patients in the acute phase of disease (day 1) showed a significant decrease in protein C amidolytic activity and antigen, anticoagulant protein S activity, and PCI antigen (P < .001). In contrast, free protein S antigen and AT-I11 levels at day 1 were normal. At day 1, a significant increase in total protein S antigen, Table 1. Coagulation Parameters for 28 Patients With MSF During the Acute Phase of the Disease (day 1) and After Remission (day 30) and 30 Healthy Subjects Patients (n = 28) Day 1 Day 30 Platelet count (109/L) vWF:Ag (%) VIII:C/vWF:Ag ratio Fibrinogen g/L FDP positive ( > 10 pg/mL)Z Factor II (YO) Factor VI1 (%) Factor IX (YO) Factor X 1%) Factor XI (%) Factor XI1 (%) Prekallikrein 1%) Healthy Subjects (n = 80) 264 f 70t 189 2 82’ 301 f 61 550 f 310* 239 2 131t 106 f 21 0.36 f 0.14’ 0.68 -c 0.25t 0.98 r 0.14 462 ? 161* 401 ? 104 278 2 49 9 1 0 106 -c 16 108 f 16 102 f 20 9 8 f 17 100 f 16 101 f 16 109 ? 22 102 f 17 98 f 20 101 2 16 9 6 2 19 9 9 2 19 108 f 19 9 9 2 15 103 L 16 96 f 20 103 18 100 -c 20 98 ? 18 95 21 101 ? 16 * * Data for all parameters except FDP positive are expressed a s mean f SD. * P < ,001 with respect to healthy subjects. t P < ,001 with respect to patients at day 1. *Number of patients with FDP positive. From www.bloodjournal.org by guest on October 28, 2014. For personal use only. VICENTE ET AL 418 Table 2. Protein C Pathway Components and Other Related Parameters in 28 Patients With MSF During the Acute Phase of the Disease (day 1) and After Remission (day 30) and 30 Healthy Normal Subjects Patients In = 28) Day 1 Day 30 Protein C antigen (%) amidolytic (%) Protein C inhibitor antigen (%) activity (%) a,AT (Yo) Protein S total (%I free (YO) anticoagulant (%) C4b-binding protein (%) AT-Ill (Yo) T:AT-Ill complex (ngimL) Healthy Subjects (n = 30) 68 f 19' 60 f 18* 102 * 19t 108 f 20t 99 f 20 103 k 19 41 20* 37 f 20' 159 f 38* 88 f 19t 85 f 19t 107 * 23t 99 f 21 97 f 19 102 2 16 119 f 19* 97 f 31 72 2 23* 135 31* 96 f 24 94 2 21 99 f 30 87 2 23t 116 f 23$ 103 f 18 4 f 3t 9 5 2 12 942 19 91 f 21 102 f 18 101 2 12 221 * 1 1 f?* lution of the disease and, on day 30, only eight patients had detectable APC:PCI complexes, ranging from 3 to 8 ng/mL. All healthy subjects had detectable levels of APC:a,AT complexes, ranging from 3 to 12 ng/mL, with a mean value of 7 ng/mL (Fig 1A). As seen in Fig lA, MSF patients at day 1 had significantly increased levels of APC:a,AT complex (mean 27 2 13 ng/mL, range 8 to 53 ng/mL) as compared with controls (P < .001). APC:a,AT complex levels were significantly decreased on day 30 (mean 14 5 7 ng/mL, range 3 to 37 ng/mL) compared with day 1 (P < .001), but remained significantly increased (P < .001) compared with normal controls (Fig 1A). PCI is a good inhibitor of KK in in vitro s t ~ d i e s . ' ~ ~ * ~ Because this enzyme may be formed in the course of infection and vascular damage?'.'' we investigated the presence of KK:PCI complexes in MSF patients. Detectable KK:PCI complex levels ( < 15 ng/mL) were not found t Data for all parameters are expressed as mean f SD. *P < ,001with respect to healthy subjects. tP < ,001with respect to patients at day 1. SP < .01 with respect to patients at day 1. C4b-binding protein, and a,AT (P < .001) was observed in MSF patients compared with healthy subjects. After 30 days of treatment (day 30), a significant increase in protein C antigen and activity was observed when compared with the values at day 1 (P < .001). Although PCI antigen and activity levels increased significantly (P < .001) at day 30 when compared with those at day 1, these values remained slightly decreased compared with normal values (P < .05). a,AT, total protein S, and C4b-binding protein decreased steadily towards normal values as the disease progressed (Table 2). AT-I11 and free protein S did not show any significant change during the evolution of the disease. Although AT-I11 levels were normal on day 1, a significant increase (P < ,001) in T:AT-I11 complexes could be detected. However, a trend of TAT-I11 towards normal values was seen on day 30 (Table 2). At the time of diagnosis (day 1),two patients had deep vein thrombosis, but there were no relevant laboratory differences compared with the other 26 patients (data not shown). Quantification of protein C activation and inactivation. Because of the remarkable decrease in protein C activity and its specific inhibitor, PCI, which suggests activation of the protein C system, we determined the levels of the complexes of APC with two physiologic inhibitors, PCI and a,AT, as well as of KK:PCI complexes. Figure 1 shows the results obtained. All healthy subjects had levels of APC:PCI complex below the detection limit of the assay used ( < 3 ng/mL) (Fig 1B). On the other hand, in the acute phase of the disease at day 1, 16 of the 28 patients studied had detectable APC:PCI complex levels, ranging from 4 to 32 ng/mL, and a mean value of 11 ng/mL (Fig 1B). These complexes decreased significantly (P < .001) with the evo- 00 0 I 00 1 0 20 0 B 0 21 00 8 000 00 0 0 1 0 60 00 t MI t L 00 20 C 0 00 00 1 0' CONTROLS 00 00 0 w 0 0 to ,DAY 1 DAV 30 PATIENTS , I Fig 1. Levels of (A) APC:a,AT, (B) APC:PCI, and (C) KK:PCI complexes in normal healthy controls and MSF patients on admission (day 1) and after remission of the disease (day 30). The continuous line indicates the detection limit of the complex assay. From www.bloodjournal.org by guest on October 28, 2014. For personal use only. PROTEIN C ACTIVATION IN SPOTTED FEVER in the healthy normal subjects, whereas 21 of the 28 MSF patients had detectable levels of KK:PCI (mean 46 2 16 ng/mL, range 21 to 86 ng/mL) (Fig 1C) during the acute phase of the disease (day 1). After remission of the disease (day 30), only five patients had detectable KK:PCI complex levels (range 24 to 33 ng/mL) (Fig 1C). Correlation between APC:inhibitor complexes and F A T-111 complexes. Figure 2 shows the correlation between APC: a,AT and T:AT-I11 complex levels (A), APC:PCI and T:AT-I11complex levels (B), and APC:a,ATand APC:PCI complex levels (C) in MSF patients during the acute phase of the disease at day 1. There was a positive correlation (r = 504, P < .005) between APC:a,AT complex levels and TAT-I11 complex levels (Fig 2A). However, no significant correlation was observed between T:AT-I11and APC: PCI complex levels (r = .138,P > S ) (Fig 2B) nor between APC:PCI levels and APC:a,AT levels (r = .309, P > . l ) (Fig 2C). Correlation between KK:PCI complexes and APCinhibitor and EAT-111 complexes. Figure 3 shows the correlation between the KK:PCI complex levels and APC:a,AT (A), APCPCI (B), or T:AT-I11 complex levels in acute MSF patients (n = 28) at day 1. There was a positive correlation (r = .438, P < .05) between KK:PCI complex levels and APC:a,ATcomplex levels and between KK:PCI and APC: PCI complex levels ( r = ,459, P < .05) but not between KEPCI and T:AT-I11complex levels ( r = .314, P > .1). Normalization ofAPC:@T complex levels. Because a,AT is an acute phase reactant and is elevated in MSF patients (Table 2), we “normalized” the values for APC:a,AT by dividing the observed level of APC:a,AT by the observed level of a,AT, and then calculated the correlation of the other complexes measured versus the “normalized” APC: a,AT levels. Again, a positive correlation was found between “normalized” APC:a,AT levels and T:AT-I11 (r = 3 1 , P < .01) and between “normalized” APC:a,AT and KK:PCI levels (r = S10, P < .Ol), and no significant correlation was found between “normalized” APC:a,AT and APC:PCI levels (r = .281,P > .1). Although there was a significant increase in the a,AT levels in MSF patients at admission (Table 2), no correlation was found between the levels of APC:a,ATand those of a,AT (data not shown). 419 60 4 E 50 \ m E 3tl 4 B0 40 30 0 20 10 0 4 E \ m C ------- 7 .em...). 0 10 . 20 30 30 r:0.309 ” 20 w x W 4 8 0 10 k PU Fig 2. (A) Correlationbetween the levels of APC:a,ATcomplex and T:AT-Ill complex in MSF patients at day 1. (B) Correlationbetween the levels of APC:PCI complex and T:AT-Ill complex in MSF patients at day 1. (C) Correlation between the levels of APC:PCI complex and APC:a,AT complex in MSF patients at day 1. For calculation of the coefficients of correlation, APC:PCI complex levels below the detection limit [ < 3 ng/mL) were consideredto be 1 ng/mL. 0 1:ATIII COMPLEXES, ng/mL DISCUSSION In the acute phase of MSF, widespread inflammatory microvasculitis is a dominant feature.’ A pronounced decrease in the VIII:C/vWF:Ag ratio secondary to endothelial damage and laboratory and clinical indications of activation of the hemostatic system, such as a significantly reduced numbers of circulating platelets and decreased protein C .. .. . . . . . . ; pa0.1 . . .. . / . . APCa,AT COMPLEXES, ng/mL C From www.bloodjournal.org by guest on October 28, 2014. For personal use only. 420 VICENTE ET AL '= 0.438 3~0.05 .. A . 0 . .. . . . 0 0 B r=0.459 P c 0.05 . 0 0 0 . 0.. 0 . rz0.314 ; PaO.1 0 .. . . 0 8 0 0 0 C e 20 40 . 60 80 100 KK:PCI COYPLEXES, nOlmL Fig 3. (A) Correlation between the levels of KK:PCI complex and APC:a,AT complex in MSF patients at day 1. (6) Correlation between the levels of KK:PCI and APC:PCI complexes in acute MSF patients. (C) Correlation between the levels of KK:PCI and T:AT-Ill complexes in MSF patients at day 1. For calculation of the coefficients of correlation, APC:PCI complex levels below the detection limit ( < 3 ng/mL) were considered to be 1 ng/mL and KK:PCI complex levels below the detection limit ( < 1 5 ng/mL) were considered to be 10 ng/mL. levels, were found in this study, and FDP was detected in some patients as well as clinical evidence of deep vein thrombosis in two of them. On the other hand, and as previously r e p ~ r t e dcoagulation ,~ factors 11, VU, IX, X, XI, and XI1 did not show significant variations, and fibrinogen levels were strikingly elevated, reflecting the behavior of fibrinogen as an acute-phase reactant (Table 1). This finding suggests that the abnormalities in the hemostatic system seen in MSF patients are due to local endothelial alterations and are not secondary to a disseminated intravascular coagulation (DIC). In fact, after rickettsial infection of endothelial cells, fourfold increased platelet attachment to the vessel wallzyand signs of platelet activation3' have been demonstrated. In the presence of an endothelial cell surface protein, TM, the rate of protein C activation increases approximately 20,OOO-f0ld.~'Thus, the small amounts of thrombin generated by the platelet activation that occur in the acute phase of rickettsial infection might accumulate on the endothelial cell surface, and the resulting thrombin-TM complex formed could trigger the activation of the anticoagulant protein C system. In fact, during the acute phase of MSF, activation of protein C system is directly demonstrated by the reduced protein C and PCI levels as well as by the appearance or increase of circulating APC:PCI and APC:a,AT complexes. During the acute phase of the disease all patients had detectable levels of APC:a,AT whereas only 16 of the 28 patients had moderate levels of APC:PCI complex. Moreover, there was a positive correlation between the APC: a,AT complex levels and the T:AT-I11 complex levels (r = ,604,P < .005) (Fig 2A), which suggests that protein C activation and complexation increase parallel to thrombin generation. However, there was no significant correlation between APC:PCI and T:AT-111 levels (Fig 2B) nor between the levels of APC:a,AT and the levels of APC:PCI (Fig 2C). The relative proportion of APC:PCI and APC:a,AT complex levels seen here in MSF patients coincides with that found in patients with thrombotic disease,'"'' but contrasts with that detected in vitro following addition of purified APC to citrated normal In that in vitro study we observed that the two types of complexes are formed at approximately the same rate. The APC complex levels seen here in MSF patients also contrast with in vivo studies in a baboon thrombotic model in which infusion of APC into baboons generated APC:PCI complex levels twice as high as the APC:a,AT levels immediately following the APC i n f ~ s i o n . ~A' .plausible ~~ explanation for the higher APC:a,AT complex/APC:PCI complex ratio seen in MSF patients as well as in patients with thrombotic disease is that the APC:PCI complexes are cleared faster than the A P C q A T complexes. Indeed, we recently found that during APC infusions into baboons, APC:PCI complexes were cleared about three times more rapidly than APC: a,AT complexes, with a t1,*of about 40 minutes versus 140 minutes, respectively." Another possibility is that enzymes generated during inflammatory vascular damage, such as thrombin and KK, could complex to and/or cleave pCI,7 ll.lZ.23.26 thus reducing PCI levels, thereby making a,AT the major inhibitor of APC. In fact, in this study we found that 21 of the 28 MSF patients in the acute phase of the disease had detectable circulating levels of KK:PCI complex, whereas this complex was not detected in any of the From www.bloodjournal.org by guest on October 28, 2014. For personal use only. PROTEIN C ACTIVATION IN SPOTTED FEVER 42 1 healthy normal subjects studied. These data provide the first evidence for in vivo occurrence of KKPCI complexes. This evidence suggests that during the acute phase of vascular damage, or during any other situation in which KK is generated, this enzyme could also modulate the in vivo activity of PCI. Plasma prekallikrein activation in rickettsiosis has been demonstrated.28xMR a o e t alMstudied volunteers in whom Rocky Mountain spotted fever developed after challenge with Rickettsia rickettsii, and observed an increase in plasma C1-inhibitor:KK complexes from 40 ng/mL before challenge to about 300 ng/mL 24 hours after the onset of the illness. Twenty-seven of the 28 patients studied showed, a t admission, APC:a,AT complex levels higher than TAT-I11 complex levels, with ratios of AE’C.a,AT levels t o that of T:AT-I11 ranging from 1.1 to 7.0. TAT-I11 (tin = 10 to 15 minutes)” is probably cleared from the circulation more rapidly than APC:a,AT complex, and this difference in half-life would explain the lower T:AT-I11levels detected in MSF patients. Several observations suggest that APC may act beneficially a t an early step in the chain of events involved in inflammation-induced c~agulopathy.~’ It has been shown that APC prevents the coagulopathy as well as the fatal outcome associated with Escherichia coli-induced shock in a baboon model of ~ e p t i c e m i aand ’ ~ that APC inhibits plateletdependent thrombosis in a baboon arterial model.’ A s indicated here, vasculitis seems to b e an important trigger for activation of t h e anticoagulant protein C system. Initially, t h e activation of protein C could be considered a defense mechanism preventing local thrombosis, and this could be the reason for the absence of occlusive thrombosis a t the level of the inflammatory vascular injury in fulminant rickettsiosis.)6 One could speculate that when the vascular injury is more severe, it may lead to inadequate production of APC that then cannot prevent t h e severe hemostatic alterations seen in the severe forms of MSF. In conclusion,our study performed in 28 MSF patients in the acute phase of the disease where a widespread microvascular injury (vasculitis) is a dominant feature has demonstrated the activation of the protein C anticoagulant system, suggesting that this pathway is intimately involved in vivo in the interaction of the coagulation and inflammatory system. These results also suggest t h e interest in screening the protein C system in clinical situations where the inflammatory process in a variety of vasculitides is involved. REFERENCES 1. Walker DH: Pathology and pathogenesis of the vasculotropic Rickettsiosis, in Walker DH (ed): Biology of Rickettsial Diseases (vol 1). Boca Raton, FL, CRC, 1988, p 115 2. Wisseman C: Selected observations on rickettsiae and their host cells, in Kazar J (ed): Rickettsiae and Rickettsial Diseases. Bratislava, Czechoslavakia,Publishing House of the Slovak Academy of Sciences, 1985, p 167 3. Montenegro MR, Mansueto S, Hegarty BC, Walker DH: The histology of “taches noires” of boutonneuse fever and demonstration of Rickettsia conorii in them by immunofluorescence. Virchows Arch [A] 400:309,1983 4. Ruiz R, Martin AM, Herrero JI, Muiioz VM, Mateos, A, Sanz F, Becares M, Querol R, Portugal J: Fiebre botonosa mediterranea. Andisis clinic0 y diagnbstico de 50 enfermos. Enf Infecc (Barcelona) 1:16, 1983 5. Vicente V, Alberca I, Ruiz R, Herrero I, Gonzalez R, Portugal J: Coagulation abnormalities in patients with Mediterranean spotted fever. J Infect Dis 153:128,1986 6. Esmon CT: The roles of protein C and thrombomodulin in the regulation of blood coagulation.J Biol Chem 2644743,1989 7. Espaiia F, Berrettini M, Griffin JH: Purification and characterization of plasma protein C inhibitor. Thromb Res 55:369, 1989 8. Gruber A, Griffin JH, Harker LA, Hanson SR: Inhibition of platelet-dependent thrombus formation by human activated protein C in a primate model. Blood 73:639,1989 9. Emerick SC, Maruyama H, Yan SB, Long GL, Harms CS, Marks CA, Mattler LE, Huss C, Comp PC, Esmon NL, Esmon CT, Bang NU: Preclinical pharmacology of activated protein C, in Holcenberg JC, Winkenhale J (eds): The Pharmacology and Toxicology of Proteins. New York, NY, Liss, 1987, p 351 10. Marlar RA,Griffin JH: Deficiency of protein C inhibitor in combined factor VNIII deficiency disease. J Clin Invest 66:1186, 1980 11. Suzuki K, Nishioka J, Hashimoto S: Protein C inhibitor: Purification from human plasma and characterization.J Biol Chem 258:163,1983 12. Suzuki K, Nishioka J, Kusumoto H, Hashimoto S: Mechanism of inhibition of activated protein C by protein C inhibitor. J Biochem 95:187,1984 13. Suzuki K, Deyashiki Y, Nishioka J, Kurachi K, Akiras M, Yamamoto S, Hashimoto S: Characterization of a cDNA for human protein C inhibitor. J Biol Chem 262:611,1987 14. Heeb MJ, Espaiia F, Griffin JH: Inhibition and complexation of activated protein C by two major inhibitors in plasma. Blood 73:446,1989 15. Heeb MJ, Griffin JH: Physiologic inhibition of human activated protein C by alpha 1-antitrypsin.J Biol Chem 263:11613, 1988 16. Tabernero D, Espaiia F, Vicente V, Estell6s A, Gilabert J, Aznar J: Protein C inhibitor and other componentsof the protein C pathway in patients with acute deep vein thrombosis during heparin treatment. Thromb Haemost 63:380,1990 17. Espaiia F, Vicente V, Tabernero D, Scharrer I, Griffin JH: Determination of plasma protein C inhibitor and of two activated protein C-inhibitor complexes in normals and in patients with intravascular coagulation and thrombotic disease. Thromb Res 59:593, 1990 18. Espaiia F, Estell6s A, Aznar J, Gilabert J: Assay of protein C in human plasma: Comparison of amidolytic, coagulation and immunochemicalassays. Thromb Res 44:771,1986 19. Fernandez JA, Estell6s A, Gilabert J, Espaiia F, Aznar J: Functional and immunologic protein S in normal pregnant women and in full term newborns. Thromb Haemost 61:474,1989 20. Espaiia F, Griffin JH: Determination of functional and antigen protein C inhibitor and its complexes with activated protein C in plasma by ELISA’s. Thromb Res 55:671,1989 21. Deutz-TerlouwPP, Ballering L, van Wijngaarden A, Bertha RM: Two ELISA’s for measurement of protein S, and their use in the laboratory diagnosis of protein S deficiency. Clin Chim Acta 186:321,1989 22. Gilabert J, Fernandez JA, Espaiia F, Aznar J, Estellts A: Physiological coagulation inhibitors (protein S , protein C and From www.bloodjournal.org by guest on October 28, 2014. For personal use only. 422 antithrombin 111) in severe preeclamptic states and in users of oral contraceptives. Thromb Res 49:319,1988 23. Espafia F, Estellts A, Griffin JH, Aznar J: Interaction of plasma kallikrein with protein C inhibitor in purified mixtures and in plasma. Thromb Haemost 65:46,1991 24. Laurel1 CB: Quantitative estimation of proteins by electrophoresis in agarose gel containing antibodies. Anal Biochem 15:45, 1966 25. Clauss A: Gerinnungsphysiologischeschenellmethode zur Bestimmung des fibrinogens. Acta Haematol (Basel) 17:237, 1957 26. Espaiia F, Griffin JH: Plasma protein C inhibitor (PCI) inhibits procoagulant and profibrinolytic enzymes. Blood 70:401, 1987 (abstr) 27. Colman RW, Edelman R, Scott CF, Gilman RH: Plasma kallikrein activation and inhibition during typhoid fever. J Clin Invest 61:287, 1978 28. Yamada T, Harber P, Pettit GW, Wing DA, Oster CN: Activation of the kallikrein-kinin system in Rocky Mountain Spotted Fever. Ann Intern Med 88:764,1978 29. Silverman DJ: Adherence of platelets to human endothelial cells infected by Rickettsia rickettsii. J Infect Dis 153:694,1986 30. Rao AK, Schapira M, Clements ML, Niewiarowski S, Budzynski AZ, Schmaier AH, Harpel PC, Blackwelder WC, VICENTE ET AL Scherrer JR, Sobel E, Colman RW: A prospective study of platelets and plasma proteolytic systems during the early stages of Rocky Mountain Spotted Fever. N Engl J Med 318:1021, 1988 31. Esmon NL, Esmon CT: Protein C and the endothelium. Semin Thromb Haemost 14:210,1988 32. Espana F, Gruber A, Kelly AB, Hanson SR, Harker LA, Griffin JH: Complexation of activated protein C (APC) with two physiologic plasma inhibitors. Circulation 78:318,1988(abstr) 33. Espafia F, Gruber A, Heeb MJ, Hanson SR, Harker LA, Griffin JH: In vivo and in vitro complexes of activated protein C with two inhibitors in baboon. Blood 77:1754,1991 34. J@rgensenLN, Lind B, Hauch 0, Leffers A, Abrecht-Beste E, Konradsen LAG: Thrombin-antithrombin 111-complex and fibrin degradation products in plasma: Surgery and postoperative deep venous thrombosis. Thromb Res 59:69,1990 35. Taylor FB, Chang A, Esmon CT, D’Angelo A, ViganoD’Angelo S, Blick KE: Protein C prevents the coagulopathic and lethal effects of Escherichia coli infusion in the baboon. J Clin Invest 79:918,1987 36. Walker DH, Hawkin HL, Hudson P: Fulminant Rocky Mountain fever. Its pathologic characteristics associated with glucose-6-phosphate dehydrogenase deficiency. Arch Pathol Lab Med 107:121,1983
© Copyright 2026