Chapter 14 Sexual Difficulties and Solutions
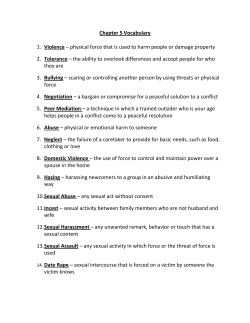
Chapter 14 Sexual Difficulties and Solutions Sexual problems are quite common • Statistically, occur more frequently in: – Younger women, older men – People w/less education • Perception of sexual problems is subjective – Not everyone experiencing a sexual problem is necessarily distressed or sexually dissatisfied Pfizer Study of Sexual Attitudes & Behaviors global survey of >26,000 people in 29 countries Types of specific sexual difficulties • In reality, these overlap considerably - problems w/desire and arousal often affect orgasm; - problems w/orgasm easily affect desire and arousal • • 3) 4) Desire-phase difficulties Excitement/arousal-phase difficulties Orgasm-phase difficulties Dyspareunia – Painful intercourse Desire-phase difficulties 1) Hypoactive sexual desire disorder (HSDD) – lack of interest both prior to sexual activity as well as lack of desire during the sexual experience • If “sexual appetite” is low, but person can become aroused/desirous after sexual experience begins, then person does not have HSDD – Used to be defined as generally low sexual appetite – In these terms, very common sexual difficulty – Contributing factors: • • • • Life stress Relationship problems Medical problems History of sexual abuse or trauma Desire-phase difficulties (cont.) 2) Dissatisfaction w/frequency of sexual activity – 2005 Global Sex Survey: 41% of men and 29% of women want sex more frequently – Couples normally have some differences in preferences re: sexual frequency (may go back & forth) • When these differences are significant source of conflict or dissatisfaction in the relationship, couple can have major difficulties 3) Sexual Aversion disorder: extreme and irrational fear of sexual activity – Thought of sexual activity can induce intense anxiety and panic Excitement-phase difficulties 1) Female Sexual Arousal Disorder: 2 types a. Genital sexual arousal disorder: persistent inability to attain or maintain lubrication-swelling response _ Subjective sexual arousal disorder: absent or diminished awareness of physical arousal • Physical signs are there, but feelings of excitement and pleasure are missing 2) Persistent Sexual Arousal Disorder – Spontaneous, intrusive, and unwanted genital arousal in the absence of sexual interest – Uncomfortable tingling, throbbing, pulsating; not relieved by orgasms--can last hours or days Excitement-phase difficulties (cont.) 3) Male erectile disorder (ED) – Consistent or recurrent inability to have or maintain an erection sufficient for sexual activity for >3 months. Quite common • 1 in 5 men over age of 20 experience ED • Incidence of ED increases with age (see graph) Orgasm-phase difficulties 1) Female orgasmic disorder – Absence, marked delay, or diminished intensity of orgasm--despite appropriate stimulation (usually clitoral) • Lack of orgasm during intercourse is not a disorder – Approx. 5-10% of adult women in U.S. – More common among women who are younger, unmarried, and have less education • Can be a learned skill, or learned w/the right partner: – One survey found that 62% of women were 18 years or older before they first experienced orgasm – Among college students, 13% of women have not had an orgasm (compared w/6% of men) – Situational female orgasmic disorder: • Refers to woman who is orgasmic when masturbating but not when stimulated by a partner Orgasm-phase difficulties 2) Male orgasmic disorder – Inability of a man to ejaculate during sexual activity – Approx. 8% of men experience this 3) Premature ejaculation – The most common male sexual difficulty – Pattern of ejaculations within 2 minutes and an inability to delay ejaculation, resulting in impairment of man’s or his partner’s pleasure – Approx. 20-30% of men worldwide age 18-59 – Men w/P.E. experience rapid arousal and often ejaculate before reaching full sexual arousal; report less enjoyment of orgasm than men w/o P.E. • Suggests some physiological component Orgasm-phase difficulties 4) Faking orgasms – Usually discussed in reference to women, though some men also fake orgasms – Reasons given: • avoid disappointing or hurting their partners • get sex over with • need for partner approval – Can lead to vicious cycle • Partner continues same method (presumably ineffective) of stimulation, which he/she believes to be effective • Creates emotional distance during physical intimacy Table 14.3 Asked college students, “Have you ever faked an orgasm?”(%) Female Heterosexual Female Lesbian/Bi Male Heterosexual Male Gay/Bi 14-A: Discussion question PART 1: Is faking an orgasm ever okay to do? Why or why not? PART 2: What do you consider premature ejaculation? Is there a time limit? If sexual activity continues after ejaculation of a male partner, does it matter if it is “premature”? What is sexual activity does not continue? Dyspareunia: Pain or discomfort during intercourse • Much more common in women (see next slide) – > 60% of women experience dyspareunia at some point • In men, dyspareunia is unusual but does occur – If foreskin is too tight (phimosis), erection can be painful – Poor hygiene of uncircumcised penis can cause infection that can irritate the glans during sexual activity – Infections in urethra, bladder, prostate gland, or seminal vesicles can cause pain w/ejaculation – Peyronie’s disease: fibrous tissue and calcium deposits develop in space above/btwn cavernous bodies of penis • Usually caused by traumatic bending of penis during intercourse • Results in pain and curvature of penis upon erection Dyspareunia in women • Situational discomfort – Inadequate arousal or lubrication – Physiological, hormonal conditions can reduce lubrication (nursing, menopause) – Vaginal infections can cause inflammation of vaginal walls that makes intercourse painful – Contraceptive foam/jelly, latex condoms/diaphragms can irritate vaginas of some women • Vulvar vestibulitis syndrome – Small, reddened area at entrance of vagina that causes severe pain – Experienced by ~10% of women – Sometimes caused by neurological problem that can be “retrained” by myofascial release, biofeedback, Dyspareunia in women (cont.) • Deep pelvic pain – During coital thrusting, may be due to jarring of the ovaries or stretching of uterine ligaments • May occur only in certain sexual positions or at certain times during a woman’s cycle (usu. ovulation or menstruation) – Endometriosis • Endometrial tissue that normally only grows on walls of uterus implants on various parts of abdominal cavity – Infections in uterus • e.g. gonorrhea – Gynecological surgeries for uterine and ovarian cancer – Torn uterine ligaments • Due to rape or problem during childbirth Dyspareunia in women (cont.) • Vaginismus – Involuntary spasmodic contractions of the muscles of the outer third of the vagina – Result in extreme pain upon insertion of a penis, or even a finger, into the vagina – Caused by a number of different possible physiological, psychological, and situational factors – Women can learn to minimize or prevent the contractions with treatment Origins of sexual difficulties: physiological factors • Vascular, hormonal, neurological problems • Poor general health, diet, and exercise – For example, body fat, especially around the abdomen, reduces testosterone levels in men, and men who are obese are 90% more likely to have ED 14.4 • Drug use – See table Physiological factors (cont.) • General chronic illness – Many different illnesses can impact sexual functioning, either due to direct impairment of nerves, hormones, or blood flow, or due to pain and fatigue suppressing desire • Diabetes: – Nerve damage and circulatory problems resulting from diabetes cause ~50% of diabetic men to have reduction or loss of capacity for erection – Women w/diabetes often have problems w/sexual desire, lubrication, and orgasm • Cancer – Chemotherapy & radiation can damage hormonal, vascular, and neurological functions necessary for sexual functioning – Nausea, fatigue, pain, negative body image after surgery – Cancers of the reproductive system usually have the worst impact on sexual functioning Physiological factors (cont.) • Multiple sclerosis (MS) – Neurological disease of the brain and spinal cord due to damage to the myelin sheath covering nerve fibers – Most MS patients experience problems w/sexual functioning, ranging from loss of sexual interest or genital sensation, reduced arousal or orgasm, or hypersensitivity to genital stimulation • Strokes: – Occur when brain tissue is destroyed as a result of blockage of blood to the brain or internal bleeding in the brain – Often result in limited mobility, altered/lost sensation, impaired verbal communication – Stroke survivors frequently report reduced sexual interest, arousal, and activity Effects of medications • Over 200 prescription and OTC medications have negative effects on sexuality • Health care practitioners don’t always discuss potential sexual side effects -- ask or do your own research • Psychiatric medications – Antidepressants: reduced sexual interest, arousal, delayed or absent orgasm in up to 60% of users – Antipsychotics: frequent loss of arousal, orgasm – Tranquilizers (valium, xanax, etc.): interfere w/orgasm • Antihypertensive medications (treat high b.p.) – Can interfere w/desire, arousal, and orgasm • Other medications – Prescription and OTC gastrointestinal, antihistamine medications can interfere w/desire, arousal, erection – Methadone can reduce desire, arousal, orgasm Disabilities • Have widely varying effects on sexual responsiveness • Cerebral palsy – Brain damage that occurs before/during birth or in early childhood – Results in mild to severe lack of muscular control – Genital sensation is unaffected, but some positions may be difficult, involuntary vaginal contractions can cause pain – Sexual adjustment depends on support from partner, social network as much as on physical possibilities • Spinal cord injury – May result in impaired physical ability for arousal and orgasm--varies considerably depending on the specific injury – Research: 86% of men and women w/SCI’s feel desire, over half experience arousal from stimulation, ~1/3 experience orgasm – Research in women has shown that the vagus nerve provides an alternate pathway from vagina/cervix to brain that bypasses the spinal cord Disabilities • Effect of spinal cord injury on erection depends on location of injury along spinal cord Disabilities (cont.) • Blindness and deafness – Can affect sexuality primarily when they interfere with learning social interaction skills, independence – Other senses can play an expanded role • Enhancement strategies for people with chronic illnesses and disabilities – Acceptance of limitations & development of remaining options – Pain control, either by minimization or treatment – Expand definition of sexuality beyond genital arousal and intercourse – Some people find that their illnesses/disabilities teach them fascinating new things about their sexuality, increase connection to partner Cultural influences • Negative childhood learning – Parents’ attitudes toward sex, level of affectionate interaction with each other – Labeling sex as sinful or shameful can contribute to sexual difficulties later in life • Sexual double standard – Research: equality of gender roles is associated with greater sexual satisfaction in men & women – Opposing sexual expectations for women and men create problems • Men feel that they should want sex all the time, that asking for guidance from their partner isn’t ‘manly’ • Women may learn to be sexually restrained for fear of being labeled a ‘slut,’ resulting in less exploration of their sexuality, not asking their partner for what they want Cultural influences (cont.) • Narrow definition of sexuality – Idea that ‘real’ sex = penile-vaginal intercourse leads to inadequate clitoral stimulation for women, places unrealistic burden on intercourse – When problems occur, too much focus is often placed on issues of erection problems, when emotional or relationship problems are very often the root cause • Performance anxiety – Usually, anxiety about not being able to achieve erection or orgasm – One transitory problem with performance can cause a vicious cycle where anxiety about repeat problems causes problems next time Individual factors • Sexual knowledge & attitudes – Awareness of our bodies and how we receive pleasure minimizes future sexual difficulties • Sexual abuse & assault – 17% of women and 12% of men were sexually abused before adolescence – 17.6% of women and 3% of men have been raped or were the victim of attempted rape – Increases likelihood of sexual difficulties later in life, affecting self-esteem, desire, arousal, and orgasm • Emotional problems – Anxiety, depression, and stress have a strong negative effect on sexuality Individual factors (cont.) • Self-image then now Individual factors (cont.) • Self-concept – Self-esteem, self-confidence correlate w/higher sexual satisfaction in women and men – Body image strongly affects sexuality • Affects women especially – Many women feel sexually inhibited b/c they are uncomfortable with their bodies • Media images of women have gotten further and further from the average size of women – Early 1980s: average model weighed 8% less than the average American woman; today, it’s 23% less • Men are increasingly affected as well – Male models/stars typically have no visible body hair and are getting ‘beefier’ – Porn gives men unrealistic idea of normal penis size Relationship factors • Unresolved resentments, trust issues, disrespect for partner • One partner feels pressured • Partners are too dependent on each other – Need balance of togetherness and separateness • Ineffective communication • Issues around pregnancy, STIs – Anxiety about unwanted, or desired pregnancy – Anxiety about contracting a STI • Problems accepting one’s sexual orientation – Homosexuals who fear societal or familial disapproval about being gay may attempt to live in heterosexual relationships despite their lack of desire for other sex Sexual enhancement/Sex therapy • Cautionary statements – self-help/sex therapy techniques described in book are often effective – professional help may be needed in the form of sex therapy, couples’ therapy, or individual therapy – see an MD to assess physical causes Sexual enhancement/Sex therapy • Self-awareness – Becoming well-acquainted with our sexual anatomy – Experimenting with masturbation to learn about sexual response • Communication – Using strategies described in Chp. 7 to improve communication about sexual activities – Learning how to tell or show partner what is desired, what type of stimulation is effective Sexual enhancement/Sex therapy (cont.) • Sensate focus – Prescribed by therapists for a number of male and female sexual difficulties – Also helpful technique to increase intimacy in couples who aren’t experiencing sexual difficulty – Principles of the technique: • Non-goal-oriented physical intimacy – Takes the pressure off of “performance” and achieving orgasm • Focus on sensation of touching your partner • Exploring sensual touching beyond the genitals • Discovering whether aspects of intimacy bring up any feelings of discomfort Specific suggestions for women • Becoming orgasmic: first alone – First: body exploration, genital self-exam, Kegels – Then: self-stimulation exercises (as described in Chp. 8) – Vibrators can help women experience orgasm for the first time so she knows what it feels like • After a few vibrator-assisted orgasms, helpful to return to manual stimulation -easier for a partner to replicate Specific suggestions for women (cont.) • Then, w/a partner – Masturbation w/partner present – Mutual body/genital exploration, then experiment w/touch, communicating their responses – Woman guides partner’s touch by placing her hand over partner’s hand on genitals – At first, to show partner what feels good – Eventually, woman may experience orgasm w/partner Specific suggestions for women • Facilitating orgasm during intercourse w/a partner – Woman can initiate movements & pressure that feel most stimulating – Woman (or partner) can also stimulate her clitoris manually or w/a vibrator during intercourse Table 14.5 (cont.) Specific suggestions for men: Strategies for delaying ejaculation • More frequent ejaculation • “Come again” • Change positions – woman-on-top, no male thrusting, to decrease muscle tension, delay ejaculation • Communication – man tells partner when to reduce or stop stimulation, then resume after a few moments • Alternative activities – intercourse is just one option • Medical treatment – Low doses of antidepressants--considerable side effects Specific suggestions for men: Strategies for delaying ejaculation (cont.) • Stop-start technique – Developed in the 1950s – Technique involves stimulation to brink of orgasm; stop, wait for sensations to decrease, start again – Man begins by working alone using masturbation – Eventually, work on technique with partner Discussion question Read the two handouts describing the sensate focus exercises and the stop-start techniques to help men delay ejaculation. What are your reactions to these exercises? Do they seem beneficial? Are there any aspects of these exercises that seem uncomfortable if you were to imagine practicing them with a partner? Specific suggestions for men: Erectile dysfunction • Reduce performance anxiety (most common cause) – Sensate focus exercises take the pressure off “goaloriented” intercourse • Then, genital stimulation other than intercourse – After man experiences full erection, partner stops stimulation, allows erection to subside – Resume genital stimulation to allow erection to return – Restores man’s confidence that erection will return • Final phase of treatment is intercourse – If man loses erection after penetration, return to oral or manual stimulation; if response is still blocked, return to nongenital sensate focus before moving forward again Erectile dysfunction (cont.) • Medical treatments – Viagra (1998); newer drugs: Levitra and Cialis • Mechanism: smooth muscle relaxation in spongy bodies of penis, increasing blood flow, resulting in erection • Similar side effects: flushing, headaches, nasal congestion • Can cause priapism (erection doesn’t subside--can cause damage to penile tissue w/o treatment): takes effect < 3 hours, requires physical stimulation, effect may depend on quality of relationship • Have increased awareness of ED • Has led to some recreational use--has led to some increase in highrisk sexual behavior in combination w/drugs & casual sex – Vasoactive medication • Common ED treatment before Viagra-like drugs • Work by relaxing smooth muscle in spongy body of penis, increasing blood flow --> erection • Required injection into penis, or suppository inserted in urethra Erectile dysfunction • Mechanical devices – Suction blood into penis and hold it there during intercourse – External vacuum devices, with penile constriction bands – Rejoyn • Penile support sleeve made from soft rubber--fits over penis to provide support necessary for intercourse (cont.) Erectile dysfunction (cont.) • Surgical treatments – Penile implants--2 types • Semirigid rods inside a silicone covering placed inside cavernous bodies of the penis (disadvantage: penis always semierect) • Inflatable prosthesis that can be pumped as needed (see below) • Surgery cannot restore sensation or ability to ejaculate if it has been lost due to medical problems (similar to Fig. 14.7 in book) Treating Hypoactive Sexual Desire • Some suggestions same as other dysfunctions – encourage erotic responses • Self-stimulation, fantasy – reduce anxiety • Sensate focus exercises – enhance sexual experiences through improved communication about which activities feel pleasurable and which do not – expand repertoire of activities • Less “goal-oriented” sexual activity • Moving beyond “genital-only” sensual/sexual activity • Therapy – Examine, resolve subconscious conflicts about pleasure – Examine whether there are unresolved relationship issues Treating Hypoactive Sexual Desire Medical treatments • Men: – Testosterone supplementation to increase desire; – Viagra to help with arousal/response • Women: – Both estrogen and testosterone therapies can increase sexual desire and arousal in postmenopausal women – Testosterone can also increase desire in premenopausal women w/below-normal testosterone levels – Zestra: oil applied to clitoris and vulva to increase sexual response – ArginMax: nutritional supplement to increase clitoral sensation, desire, vaginal lubrication, orgasm frequency – Bremelanotide: inhalant that acts on neural pathways to increase desire and genital arousal--still in research phase – Creams containing alprostadil, prostaglandins, or L-arginine to inrease blood flow to genitals, enhance arousal and orgasm Seeking Professional Assistance • What happens in therapy? – identify & clarify problems & goals – medical, sexual, relationship history – often given homework – NEVER includes sex with therapist • Selecting a therapist – referral from trusted source (some listed in text) – ask about credentials, training, & experience – interview: practicalities & "fit"
© Copyright 2026