LGBT Health Health of Lesbian/Bisexual Women and
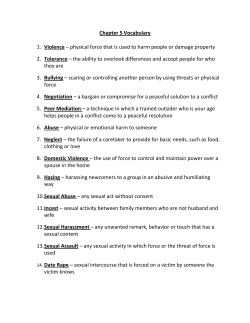
LGBT Health Health of Lesbian/Bisexual Women and Trans Men May 3rd, 2013 UNC Chapel Hill School of Medicine LGBT sensitivity is important for physicians as a matter of policy and of professionalism with coworkers and patients. LGBT patients have specific health concerns and experience health disparities, primarily due to stigma, discrimination, and barriers to health care. In order to provide effective health care to LGBT patients, physicians should be familiar with these concerns, disparities, and the population. A review Attraction Biology Gender Sexuality LGBT language gay – primarily attracted to same gender lesbian – woman primarily attracted to other women bisexual – person attracted to both men and women queer, as a sexual orientation – person attracted to one or more genders along the spectrum queer community – umbrella term for gender/sexual minorities transgender – identifies as gender different from assigned gender transwoman – assigned male, identifies female (MTF) transman – assigned female, identifies male (FTM) In this session Health concerns and disparities in lesbian/bisexual women Health care of transmen Education on topics specific to these groups This session is not intended to establish stereotypes of lesbian or transgender patients. We will discuss patterns shown so far in the (limited) research. It is up to you, the physician, to create an environment in which your patient can disclose to you, and then to use this information to assess what is important for your patient. Case #1: 14yo female patient coming in for annual check-up. You have noted that she started experiencing puberty last year. What questions would you ask about her sexuality, and how? Defining Lesbian Attraction? Behavior? Identity is the definition commonly used in epidemiological research and most affirming for your patient. 1-5% of the female population 70% are WSW, 30% are WSMW Diverse in race, age, education, income, geography Lesbian youth Increased risk of sexual, psych, physical abuse More likely to report early drinking 4x higher likelihood of substance use Twice as likely to attempt suicide Protective factors include family connectedness, other adult caring, school safety – similar protective factors to other populations Lesbian youth • • • Approaching sexual orientation (as a physician): Non-assuming Non-judgmental Emphasizing confidentiality Going forward: Sexual identity can still change Should still get HPV vaccine as recommended Still need safer sex and contraceptive education Sexual function Sexual behaviors in WSW (and largely for WSM): Oral-vaginal genital-genital digital-vaginal vaginal toys, oral-anal Anal toys digital-anal BDSM Sexual function (the other side) 23% of lesbians with sexual dysfunction - only 3% of them saw a physician. Common to all women: May have decreases in desire, arousal, lubrication, pleasure, orgasm with increased age. Effects are less pronounced with higher relationship satisfaction. Case #2: 25yo female patient comes in with odorous, white vaginal discharge. What questions do you ask about her sexual history/behavior? STIs in lesbians Common STIs – BV, chlamydia, HSV, HPV, lice, trich Less common – gonorrhea, hep, HIV, syphilis Risk factors for BV – smoking, # partners, partner with BV, shared sex toy, receptive oral-anal - 23% concordance of BV with partner. Safer sex tips Avoiding blood, vaginal fluid, breastmilk. Wearing gloves or fingercots. Using condoms or cleaning sex toys. Dental dams or plastic wrap. IPV in lesbian relationships 30-40% of lesbians have experienced IPV – compared to 35% of women in the general population The perpetrator is often older. - Pattern of being perpetrator or victim may change. Additional hiding or intimidation if victim is not out – may be more prevalent in first relationships after coming out Lesbians tend to go to support groups, counseling, and shelters, but least frequently to neighbors, attorneys, physicians. Case #3: 28yo female patient comes in with fatigue, and she thinks it’s because she wakes up early in the morning and can’t fall back asleep. What other clinical information would you like? What screening questions would you ask? What parts of her social history would you inquire about? Mental health Conflicting evidence on how prevalence of depression in lesbians compares to general population. Some studies report higher self-esteem in lesbians compared to straight women. Bisexual women often have poorer mental health more often than lesbian and heterosexual women. Alcohol use Bars in the lesbian community – similar to the role of bars in other communities, can have both positive and negative outcomes For lesbians who do seek help with alcoholism, 74% of relied on additional supports outside of AA, but: Many alcohol treatment centers do not offer LGBTspecific services or have negative attitudes towards LGBT patients, or are not familiar with LGBT issues like internalized homophobia Need to consider when referring patients Smoking Higher prevalence of smoking in lesbian/bisexual women (25-30%) compared to straight women (15-20%) May be associated with advertisements targeted to LGBT community Often begins during adolescence when many lesbians are coming out Nutrition/exercise Being overweight in the lesbian community may result from unclear mechanisms that require individualized patient counseling Unclear mechanisms – greater acceptance of large body size, social induction, rejection of “thin” aesthetic Cancer Lower rates of getting Pap smears, clinical breast exams, and maybe mammograms Breast cancer risks smoking, nulliparity, obesity (postmeno), alcohol, no breastfeeding Ovarian cancer risks increased BMI, nulliparity, no OCP Endometrial cancer risks increased BMI, nulliparity Cervical cancer risks HPV, smoking Case #4: 35yo female patient says she doesn’t feel like getting a Pap smear since she’s been monogamous with her female partner for over 10 years. Would you recommend a Pap smear? How would you counsel her? Reproductive health Some lesbians do want birth control. 15-30% are sexually active with men. Increased rate of unintended pregnancy in lesbian and questioning female youth. (Review: Don’t make assumptions) • • • Oral contraceptives may decrease risk of ovarian/uterine cancer, and can also treat endometriosis, PCOS, dysmenorrhea. Pregnancy options Studies show: 50% of lesbians want to be parents. 30% of these become biological mothers. Insemination by known or unknown donor (Intrauterine > cervical ) Intercourse Co-maternity Adoption/foster Planning for pregnancy should be encouraged for ALL women. Blood work (rubella, HIV, CF) Prenatal vitamins 3mo before conception Decisions about various parental roles Legal advice Pregnancy difficulty Lesbians postpone childbearing longer, resulting in increased miscarriages, abnormal karyotypes, decreased fertility. Recommended that lesbian couples using IUI who fail to impregnate after 3-6 months see an infertility specialist Increased incidence of postpartum depression. Case #5: 28yo patient wants to have a child with her female partner, but they want to wait 5+ years until they’re completely ready. What are their options? How would you counsel them? Hospital/ end-of-life care for lesbians As of 2008, North Carolina allows patients to designate visitors regardless of legal status Is the law always followed? Helpful documentation Durable health care power of attorney (true for any non-married couples) Out-of-hospital DNR form Last will and testament Instructions in event of death Hospice and nursing facility care: concern about homophobia, treatment, discrimination, child custody, etc. 25% of survivors experienced complicated grief over loss of a life-partner, especially if not out. - Compared to only 6-15% of survivors in general population Gender expression Reversible options: Clothing/hair/make-up Voice/manner Prosthetics/binders Name/pronoun Does not require a medical provider or expensive care; may not be as "passable," may still feel discordant ‘Real-life experience’ (RLE) usually required for further therapy. e.g., 3mo rec before hormones, 3mo req before top surgery, 1 yr req before bottom Guidelines for Transition World Professional Association for Transgender Health (WPATH) formerly Harry Benjamin Internat’l Gender Dysphoria Association (HBIGDA) Vancouver Coastal Health Trans Care Project The Endocrine Society Options for Transition Gender expression Hormones Surgery Chest (top) Genital (bottom) Cosmetic Vocal Psychotherapy Often required or recommended before hormone therapy or surgery Intended to ensure readiness and minimize regret after surgery, and establish relationship with health care. Assess state and development of gender identity, gender concerns, co-existing problems. Explore options for gender expression, identity management, social support. Diagnosis of Gender Identity Disorder may be required for further therapy - Pathologizes preference for gender dysphoria Often perceived as a hoop to jump through, loss of autonomy, transphobic discrimination; but can be a source of support during a serious life change. Testosterone • • • • • • Increase muscle, reduce fat Increase facial hair/acne Increase libido, Enlarge clitoris, vaginal/breast atrophy Decrease fertility, cease menstruation Deepen voice Side Effects • • • • • • Hormone therapy for FTM Excessive acne Weight gain, salt retention Sleep Apnea Increased RBC/polycythemia Decreased HDL, variable effects on LDL Scalp hair loss Hormone therapy for FTM • • • • • Administered through injections, gels, patches, pills Pros: • Closer match between appearance and self-perception with identity • Reversible Cons: • Expensive • Continual treatment • Genitals can still be a source of dysphoria Highly recommended to consult a medical provider before/during Adolescents can take puberty-delaying hormones before deciding hormone therapy or surgery Surgeries Gender Affirmation, Sex Reassignment, Genital Reconstruction Breast removal or reduction. Hysterectomy/oophorectomy, vaginectomy, metaidioplasty, phalloplasty, scrotoplasty Best "treatment" for gender identity disorder Cons: expensive, irreversible, surgeons/surgeries are not perfect (loss of sensation) Rhinoplasty Chin/jaw implants Pectoral implants Liposuction Surgeries Elective Bilateral Mastectomy – Removal or reduction of the breasts (reduction mammoplasty, “top surgery”) Incision made near nipple, tissue and fat removed from under the skin to shape into “masculine” chest Option to have skin grafted from existing nipple to create a new “male-like” nipple Few complications, length varies per patient Reduction mammoplasty is often all a FTM needs to comfortably assume a new gender role and pass in society. Surgeries Metoidioplasty – Creation of a penis by extending the clitoris that has been significantly enlarged by testosterone hormone use Skin around the clitoris is removed so that the clitoris can extend from the pubic region and appear as a penis. The resulting penis is smaller than the average size of an adult male penis and its use in sexual intercourse is limited. Option to have the urethra lengthened, which makes it possible to urinate while standing. This requires removal of the vagina. Fat of the pubic area is typically removed and the skin pulled tighter around the area, creating a more male-like appearance. The vaginal opening is closed and the skin of the vaginal labia (lips) is used to create a scrotum. Inflatable expanders are placed in the scrotum either during or after surgery in order to expand the skin of the newly created scrotum. Once expanded, the scrotum can accommodate testicle implants. Surgeries Phalloplasty (free flap phalloplasty) Constructing a penis from the inner forearm skin (nondominant side) and vaginal tissue Forearm skin is grafted along with its nerves, arteries, and veins and formed around a plastic catheter tube, which will serve as the urethra and allow for urination. The forearm skin is used to create the shaft, glans (head), and urethra. Nerves of the clitoris are attached to the grafted nerves and will grow into the penis after surgery. Skin and tissue of the vaginal labia is used to create a scrotum. The procedure may take 3 hours or more. After 6 to 9 months of healthy recovery, cosmetic testicle implants can be inserted in the scrotum. Erectile implants, those used in men with impotence (erectile dysfunction), can be added to achieve erection in the new penis. Hardening of the urinary tract and tissue death in the new penis are complications of phalloplasty. Health Care of Transmen Assessing for readiness or desire for transition with hormones or surgery Monitoring hormone therapy and side fx Ask about how they’re acquiring and injecting. May still need contraceptive education if having sex with male-bodied persons Should still be getting Pap smears if the patient has a cervix Screening for drug/alcohol use, mental health, STI, violence etc. Trans persons are at even higher risk. Tips for gyn exam of transman Do not assume anything about the patient’s sexual orientation or behavior. Tips for gyn exam of transman Split the exam into two parts - clothed interview and gowned physical, maybe even as two appointments. Tips for gyn exam of transman Allow them to bring a friend for support, distraction. Tips for gyn exam of transman Ask if they have had penetrative sex before they may like to try using the speculum on themselves first. Give the patient time to see pictures of a Pap being done, hold a speculum, etc. Tips for gyn exam of transman Be sensitive and respectful about the words you use. Ask how the patient refers to his genitals. ‘internal/external genitals’ instead of cervix and labia, ‘healthy ’ or ‘normal for you’ If the patient does not want an internal exam, you can still perform an external exam, provide education about cervical health, and build a trusting relationship. Tips for gyn exam of transman Don’t turn the patient into a teachable moment for you or your students. Tips for gyn exam of transman Transmen on testosterone may have an enlarged clitoris and atrophic cervix and fewer secretions. Include a note for the lab with any gyn samples. Case #6: A new patient comes into your office for a check-up. You notice that they’ve circled “M” under “Gender: M/F” on your intake form. Something about your patient’s appearance makes you think they might be transgender. Does it matter? How do you ask? What is the appropriate care for this patient? Creating a welcoming environment Office and hospital environment Posters, brochures, symbols, restrooms Office and hospital staff Trainings, LGBT staff, non-discrimination Inclusive forms and language Patient-physician interaction Rapport, sensitivity, openness, confidentiality, non-judgment Providing resources and referrals Inclusive forms and language Forms “Relationship,” “partner,” “parent or guardian,” fill-in for gender/ orientation, asking gender identity and birth sex and pronoun Non-assuming, non-judgmental Gender-neutral, non-heteronormative Mirror the patient’s words. Take-home messages Lesbian/bisexual and transmale communities have specific health disparities and concerns, possibly sharing a common cause. Physicians should be aware of these issues in order to serve their patients better. It is important for these communities to feel comfortable accessing needed health care and to disclose their gender/sexual identity. Some resources GLMA, Fenway Health Institute, National Coalition for LGBT Health Lesbian Health & Research Center Lesbian Health 101: A Clinician’s Guide Suzanne Dibble RN and Patricia Robertson MD National Center for Lesbian Rights (legal) LesbianSTD.com (safer sex) Checkitout.ca and Checkitoutguys.ca (Pap smears) Center of Excellence for Transgender Health Acknowledgements Alice Chuang, Krishna Foust (Ob/gyn rotation) Terri Phoenix, Danny Depuy (UNC LGBTQ) Dinushika Mohottige, Perry Tsai (QSA) Questions? Abigail Liberty [email protected]
© Copyright 2026