The Beauty of Change WRSU Customer Service
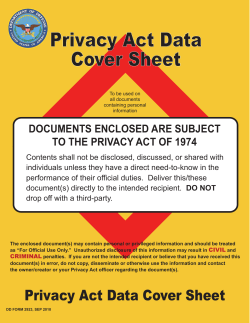
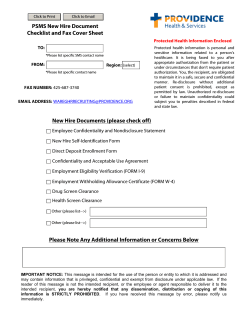
WRSU Customer Service The Beauty of Change Privacy and Confidentiality Foreword As health care workers we see and hear confidential information every day. We are entrusted with patients’ health information solely to be of service to that patient. We will go over HIPPA, the Federal endorsement of all health care employees responsibility to patients. We’ll cover both benefits and consequences. Provide health care services for 18,000 Users Close knit community with many hospital staff and residents being interrelated: – Family – Friends – Acquaintances What is Privacy and Confidentiality? Basic rights of every person Privacy is the right of an individual to keep personal information from being disclosed Confidentiality is how we as health care providers/employees treat private information once we and others receive it What is Privacy and Confidentiality? All health care providers/employees have an ethical and legal obligation to maintain the patients’ privacy and confidentiality Protecting patients’ confidentiality has always been each employee’s responsibility Health Insurance Portability and Accountability Act of 1996 (HIPAA) Standards for: Privacy of Individual Identifiable Health Information”. Provides National standards for protecting PHI. Regulates how to “use and disclose certain PHI. Gives patients more protection & control over their PHI. Sets boundaries on the use and release of health records. Establishes appropriate safeguards protecting the privacy of PHI. Bill Tibbitts: IHS Privacy Act Officer Why do we have HIPAA? Protects the patient’s rights to the confidentiality of their medical record and gives them more control of how info is shared Why do we have HIPAA? Protects electronic transmission of certain health information as well as certain patient identifiers Created federal civil and criminal penalties for breaking the confidentiality of a patient Privacy and Confidentiality Issues Patients expect that health care providers will maintain confidentiality Privacy and Confidentiality Issues Need to balance patient safety and treatment with respect for patient confidentiality Privacy and Confidentiality Issues Remember that info may sometimes need to be shared on a “need to know” basis Patient can say it is okay to share information with other family members but be sure to document you received verbal approval Privacy and Confidentiality Issues Rural Settings have additional problems of maintaining privacy and confidentiality – Inter-relatedness and familiarity of patients, residents, and staff – No big city anonymity – More parochial thinking Consequences What happens when the health care employees do not protect the confidentiality of patients? Consequences TRUST in the health care system is broken Consequences Results in ineffective medical care Unable to obtain an accurate medical history Reluctance to share medical information with staff Reluctant to come to hospital for care Consequences Possible fines for Hospital Staff termination Hospital loses accreditation Every Health Care Employee’s Role Promote and advocate patient’s rights Every Health Care Employee’s Role Set the example: closing medical records close out computer when not in use share medical info sparingly on a “need to know” basis Every Health Care Employee’s Role Remind your colleagues of the need to respect patient privacy & confidentiality Other Strategies Remind others that it is the responsibility of all employees to keep patient information totally confidential Strategies Share patient information on a “need to know” basis according to medical necessity Does this person really need to know this information to do their job? If it were my medical information what would I want? Strategies Messages or letters for patients Leave message in sealed envelope marked confidential Mark letters confidential Strategies Paper documents Keep confidential papers, reports, computer disks, and data in a secure place Retrieve confidential papers from fax machines, copier, and other publicly accessible places as quickly as possible Always tear or shred any unneeded documents, notes, etc. containing patient information Strategies Conversations: In person and on the phone Avoid discussing patients in areas where you can be overheard Always identify the person you are talking to If a patient, ask for two identifiers Confidentiality can be broken: When a patient gives consent. When a patient is a danger to himself or others. When a patient has a communicable disease. – Process must be followed. – Ethical justification of the prevention of harm to others must be clear. Implications for Health Care Providers You are asked by family members, friends, and other employees how a patient is doing? Harmless or not? Test Your Knowledge Let’s see how well we do! Tell if the following statements are true or false. Good Luck! Test Your Knowledge Patients may be more likely to share information with health-care workers if they know it will be kept private. Failure to protect patient confidentiality can lead to legal and disciplinary action. Recent developments in health care make safeguarding confidentiality easier. Test Your Knowledge Conversations between patients and health-care workers are confidential. A facility can NEVER release a patient’s name without that patient’s consent. A court has the power to force disclosure of confidential patient information. In general, close friends and family have a right to a patient’s information. Test Your Knowledge Policies and laws regarding patient confidentiality vary widely. It isn’t always necessary to share patient information with a minor’s parent. Patient with AIDS and HIV have no right to patient confidentiality. Summary As health care employees, we see and hear confidential information every day Health information belongs to the patient It can only be shared on a “needs to know” basis Summary If you have to ask yourself whether this information can be shared, usually the answer is NO! Remember Health care employees are entrusted with patients’ health information solely to be of service to that patient.
© Copyright 2026