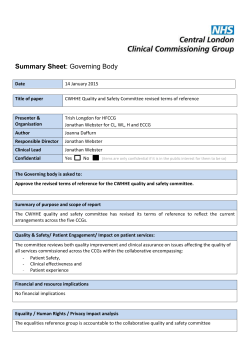
Governing Body Papers — January 2015 (pdf | 7.1 MB)
CLINICAL COMMISSIONING GROUP (CCG) GOVERNING BODY MEETING Wednesday 14th January 2015 at 1 pm Meeting Rooms 1 and 2, Blackburn Central Library Town Hall Street, Blackburn BB2 1AG AGENDA Item No: Agenda Item Member Responsible PUBLIC PARTICIPATION 1. Chairman’s Welcome Report Mr Joe Slater 2. Apologies for Absence and Confirmation of Quoracy Mr Joe Slater 3. Mr Joe Slater 4. Declarations of Interest relating to items on the agenda Questions from Members of the Public 5. Engage – Sexual Exploitation Assurance 6. Patient Story PART 1 BUSINESS (APPROXIMATELY 2 PM) 7. Minutes of the Meeting Held on 5th November 2014 7.1 Extract from Part 2 of the Minutes of the Meeting held on 5th November 2014 Mr Joe Slater Mr Nick McPartlan – Engage Team/ Ms Linda Clegg – Director of Children’s Services Mr Stuart Sheridan/ Mrs Jeanette Pearson Presentation Mr Joe Slater Attached Attached Presentation 8. 8.1 Matters Arising Action Matrix Mr Joe Slater 9. Clinical Chief Officer’s Report Dr Chris Clayton Attached 10. Chief Finance Officer’s Report Mr Roger Parr Attached 11. Contract Performance Report Mr Roger Parr Attached 12. Quality and Performance Exception Report Mrs Kim Smith Attached 13. Stakeholder Support for Healthwatch Blackburn with Darwen and Healthwatch Lancashire Mr David Rogers Deferred 14. Co-Commissioning Primary Care Update Mrs Julie Kenyon 15. Intensive Support to People Living at Home Mrs Alison Shaw Attached 16. Healthier Lancashire Purpose Document Dr Chris Clayton Attached Attached Page 1 of 2 17. Managing Conflicts of Interest – Revised Conflicts of Interest Policy 18. Lancashire Collaborative Commissioning Board Terms of Reference and Membership STRATEGY 19. Planning Guidance – 2015/16 Year 2 Update FOR INFORMATION 20. Governing Body Sub-Committees and Groups’ Summary 21. Any Other Business 22. Date and Time of Next Meeting: Wednesday 4th March 2015 in Meeting Rooms 1 and 2, Blackburn Central Library, Town Hall Street, Blackburn BB2 1AG Mr Iain Fletcher Attached Mr Roger Parr Attached Mr Roger Parr Attached Mr Iain Fletcher Attached All Mr Joe Slater EXCLUSION OF THE PRESS AND PUBLIC – ‘That representatives of the press and other members of the public be excluded from the remainder of the meeting having regard to the confidential nature of the business to be transacted, publicity on which would be prejudicial to the public interest’ (Section1(2)Public Bodies(Admission to Meetings)Act 1960) PART 2 (APPROXIMATELY 3.15 PM) A/15 Minutes of Part 2 of the meeting held on 5th November 2014 B/15 B/15.1 Mr Joe Slater Attached Matters Arising Action Matrix Mr Joe Slater C/15 Independent Investigation Report Mrs Kim Smith Attached D/15 Stakeholder Letter Dr Chris Clayton Attached E/15 Out of Hours Service Dr Chris Clayton Attached F/15 Any Other Business Mr Joe Slater Attached Page 2 of 2 Subject to approval at the next meeting CLINICAL COMMISSIONING GROUP (CCG) Item 7 Minutes of the Governing Body Meeting held on Wednesday 5th November 2014 in Rooms 1 and 2, Blackburn Central Library, Town Hall Street, Blackburn BB2 1AG PRESENT: Mr Joe Slater Mr Roger Parr Dr Pervez Muzaffar Mr Paul Hinnigan Dr Penny Morris Mrs Debbie Nixon Dr Malcolm Ridgway Dr Adam Black Mrs Anne Asher Chairman (Chair) Chief Finance Officer Executive Member Lay Member - Governance Executive Member Chief Operating Officer Clinical Director for Quality and Effectiveness Executive Member (Part) Lay Member - Nurse Representative IN ATTENDANCE: Mr Iain Fletcher Dr Gifford Kerr Mr Peter Sellars Mrs Pauline Milligan Min No: 14.076 Head of Corporate Business Consultant in Public Health, Blackburn with Darwen Borough Council Interim Commissioning Manager Corporate Support Officer (minutes) Chairman’s Welcome The Chair opened the meeting by welcoming all attendees and members of the public. He introduced himself and gave a short briefing with regard to the content of the agenda, meeting protocol and housekeeping. 14.077 Apologies for Absence and Confirmation of Quoracy Apologies for Absence had been received in respect of: Dr Chris Clayton Dr Nigel Horsfield Dr Zaki Patel Mr Dominic Harrison Dr Tom Phillips Clinical Chief Officer Lay Member - Secondary Care Doctor (Retired) Executive Member Director of Public Health, Blackburn with Darwen Borough Council Executive Member The meeting was confirmed as quorate. 14.078 Declarations of Interest Relating to Items on the Agenda The General Practitioners (GPs) at the meeting declared a generic interest with regard to Item 13 – Primary Care Strategy and Item 14 – Co-commissioning Primary Care Update. Page 1 of 10 The Chair reminded Governing Body (GB) members and members of the public that they should, if appropriate, make a declaration should a conflict emerge during the meeting and these would be recorded against the relevant agenda item. 14.079 Questions from Members of the Public The Chair reminded those attending the meeting that the CCG had produced a protocol, published on its website, in respect of members of the public who wished to ask questions or make statements at GB meetings. The protocol requested that the CCG received advanced notification of the question by 5 pm on the Monday prior to the meeting so that an appropriate response could be prepared. The Chairman stated that he was aware that a member of the public wished to ask a question despite there being no advance notification. He added that depending on the nature of the question, the CCG may need time to gather any information required and provide a written response following the meeting. Q I understand that Blackburn with Darwen (BwD) will be used as a pilot area for the Government’s care.data experience yet not a single patient in BwD had been informed that this was happening. I would have thought as a CCG you would at least require your General Practitioners (GPs) to let their patients know. Q This is a meeting in public but you do allow the public to actually participate. East Lancashire Hospitals NHS Trust (ELHT) does not. It is a waste of time sitting there like a rag doll listening to them. Could this CCG please take up the issue of making ELHT hold a meeting in public that actually allows the public to participate? A The Chair: Thank you very much for those questions. With regards to the latter question, I will discuss the matter with the Chair of ELHT when I next meet with her. A Mr Roger Parr, Chief Finance Officer: In reference to the first question raised regarding care.data, the CCG will be a pathfinder. We are in the very early stages at the moment. What we will be doing within the next few weeks is contacting GP Practices to find out which GP Practices want to participate. When that happens we will then be contacting their patients to involve them in things such as the content and design of materials; how we are going to communicate to individuals with regards to the data and the processing that needs to happen. So, it is in hand. There is a Communications and Engagement Plan that will come along with this, it’s just that we are in the early stages at the moment. The Chair invited any further comments from the GPs present at the meeting. There were no further comments. 14.080 Due North Report The Chair introduced Dr Gifford Kerr, Consultant in Public Health, BwD Borough Council who provided a presentation on the Due North report which was published as a result of an enquiry into health equity for the North; commissioned by Public Health England in February 2014 and launched in September. The report had been presented to the BwD Health and Well-being Board (H&WBB) and it had since been agreed that the information was of sufficient interest to be shared with a wider section of the public, hence the CCG’s decision to bring the presentation to its GB meeting. Page 2 of 10 Dr Kerr outlined the aim of the enquiry, which was to address the social inequalities in the North of England. Dr Kerr drew members’ attention to the differences in life expectancy throughout the United Kingdom and it was noted that for the poorest 20% life expectancy has improved more slowly in the North than the rest of England over the last 10 years. Dr Kerr referred to some of the policy drivers which resulted in inequalities, potential solutions and recommendations for the North as a whole and central Government: • Economic development and living conditions Recommendation 1: Tackle poverty and economic inequality within the North and between the North and the rest of England • Development in early childhood Recommendation 2: Promote healthy development in early childhood • Devolution and democratic renewal Recommendation 3: Share power over resources and increase the influence that the public has on how resources are used to improve the determinants of health • The role of the health sector Recommendation 4: Strengthen the role of the health sector in promoting health equity Questions and answers followed. RESOLVED: That the Governing Body noted the content of the report. 14.081 Minutes of the Meeting held on 3rd September 2014 The minutes of the meeting were accepted as an accurate record. RESOLVED: That the Minutes of the Meeting held on 3rd September 2014 were approved as a correct record. 14.081.1 Extract of Part 2 of the Minutes of the Meeting held on 3rd September 2014 The extract of Part 2 of the minutes of the meeting was accepted as an accurate record. RESOLVED: That the Extract of Part 2 of the Minutes of the Meeting held on 3rd September 2014 was approved as a correct record. Page 3 of 10 14.082 Matters Arising/Action Matrix Minute 14.065 Contract Performance Report Mrs Debbie Nixon reported that the issue related to the overall performance of the North West Ambulance Service (NWAS) and its failure to hit the target and was not specifically related to the BwD CCG area. Mrs Nixon had fed back the comments from the GB relating to NWAS performance to Blackpool CCG, as the Lead Commissioner for ambulance services. Mrs Nixon reported that there was an Action Plan in place, which is monitored via the NWAS Commissioning Group and this information is fed back through the Collaborative Commissioning Group. Mrs Nixon added that NWAS had written to CCGs and Primary Care recently indicating that the service was under pressure due to a significant increase in activity. She identified several initiatives which were in place within BwD to reduce the pressure on ambulance services, e.g. the Acute Visiting Scheme and the Intensive Support at Home Service. 14.083 Clinical Chief Officer’s Report Dr Malcolm Ridgway presented the Clinical Chief Officer’s Report in the absence of Dr Chris Clayton and highlighted key items of national and local interest. Items of note related to: • • • • • • • • • • • • • • • Achieving Better Access to Mental Health Services by 2020 Government Response to Ebola H&WBBs NHS England appointments The NHS Five Year Forward Review Improving Eye Health and Reducing Sight Loss – a ‘call to action’ Healthwatch Care Quality Commission Inspections of GP Practices Making Every Adult Matter (MEAM) Lancashire Health Expo BwD CCG Annual General Meeting Pennine Lancashire Mental Health Unit ELHT Health Service Journal Awards Care.data Pathfinders Mrs Nixon provided an update on the CCG’s submission of plans regarding the Better Care Fund. The CCG had received national feedback earlier in the week and was very pleased to have received a category grading of ‘approved with some support’. Questions and answers followed. ACTION: It was agreed that developments related to the NHS Five Year Forward Review would be presented to the next meeting of the GB by Mrs Debbie Nixon. ACTION: The Chair agreed to feedback comments related to the communication and engagement of plans for the Pennine Lancashire Mental Health Unit to Lancashire Care NHS Foundation Trust (LCFT). RESOLVED: That the Governing Body noted the content of the report. Page 4 of 10 14.084 Chief Finance Officer’s Report Mr Roger Parr presented the Finance Report which provided details of the CCG’s overall position at the end of September 2014. Mr Parr drew members’ attention to actions from the last meeting indicated in the Action Matrix and highlighted Appendix C of the report which now indicated the type of contracts. He informed the meeting that he had discussed the scenarios and risks with Mr Paul Hinnigan, Chair, Audit Committee, as this detailed scenario planning was not contained within the Executive Financial Summary. The current revenue position remains on plan to deliver the planned year end surplus of £2,307k. Year to date the CCG is reporting a cumulative breakeven position. Mr Parr highlighted the position within healthcare commissioning from providers and reported a year-end forecast overspend of £3,378k. Primary Care Services were reporting a forecast underspend of £104k and it was noted that year to date there had been a deterioration in the position related to primary care prescribing, which was being monitored. Corporate Services were reporting a probable year-end underspend of £63k. Mr Parr drew members’ attention to the highlighted risks. Questions and answers followed. RESOLVED: That the Governing Body noted: i. the content of the report ii. the overall position of the CCG at the end of September 2014 iii. the risks highlighted within the report iv. the detailed appendices supporting the narrative 14.085 Contract Performance Report Mr Roger Parr presented the Contract Performance Report, which gave the GB an update on the activity performance of the major commissioned services of the CCG as at Month 5, August 2014. Mr Roger Parr drew members’ attention to key information: • • • LCFT – Mental Health – which continued to show a reduction in admissions across Lancashire and a reduction in bed days (page 2) Referrals – the position overall is down when compared to the same period last year (page 3) o Specialty levels – there was an increase in Ear, Nose and Throat (ENT) referrals and investigation revealed that this was related to urgent ENT referrals. o Ophthalmology continued to be considerably under plan. It was noted that this was across the whole of East Lancashire and not specifically BwD and was being investigated with ELHT. Contract Performance (page 3) – indicated a similar position to previous months with pressures in Accident and Emergency (A&E) and elective activity but there were reductions in activity in non-electives and out-patients. Page 5 of 10 • • • • ELHT Waiting Lists (page 5) – the total size of the waiting list had decreased by 14 patients in August. o Referral to Treatment (RTT) – a contract variation had been agreed with ELHT with regards to the funding associated to delivering the 18 weeks RTT target. 36 Week Waiters (page 5) – 11 patients are on an incomplete pathway waiting over 36 weeks. There were no waiters over 52 weeks. Ambulance Contract (page 5) – the ambulance contract for BwD was delivering its target but acknowledged that NWAS overall was not hitting the target (as referred to by Mrs Nixon under 14.082). LCFT – Community Services (page 6) – Mr Parr referred to the Action Matrix and reported that the CCG was in detailed discussions with LCFT regarding the quality of community data. Questions and answers followed. ACTION: Following a comment from a member of the public Mr Parr agreed to consider a request to include data related to Patient Transport Services in future reports. RESOLVED: That the Governing Body noted the content of the report and the supporting appendices. 14.086 Quality and Performance Exception Report Dr Malcolm Ridgway, Clinical Director for Quality and Effectiveness, presented the GB with an update on the quality and performance exception report for month 5; the full report being regularly presented to the Quality, Performance and Effectiveness Committee (QPEC). Dr Ridgway drew members’ attention to key information: • • LCFT – Mental Health Service o Improving Access to Psychological Therapies (page 1) – Dr Ridgway referred to the prevalence target, i.e. how many people ought to be referred to the service and how many people were actually referred to the service and the expectation target for this, which was 15% annually. Dr Ridgway reported a drop in the figure for the month of August but it was predicted that the target would be reached by the end of the year. o Memory Assessment Service (page 1) – the target had not been reached and work was ongoing to improve the service. o Care Programme Approach (CPA) 7 day follow-up (page 1) – the operating standard referred to patients with more serious mental health problems being followed up following discharge. Blackpool was the only area for which the CPA was failing on a year to date position. ELHT o 18 Week RTT (page 2) – there were 3 areas which were failing to achieve the standard but these were being monitored closely by the Lead Commissioner, East Lancashire CCG. o A&E 4 Hour Target (page 2) – the target is being reached cumulatively for the year but would be closely monitored. o Clostridium Difficile (page 2) – there have been an increase in cases but it is hoped to still hit the target for the year. o Stroke 4 Hour (page 2) – the figures have continued to show gradual Page 6 of 10 improvement Mortality (page 3) – the figure showed a slight deterioration but would not trigger the CCG as an outlier. There was a lot of work taking place to review mortality rates. o Friends and Family Test (page 3) – the criteria had changed but, when compared to other local A&E Trusts, ELHT still performs poorly. Calderstones Partnership Foundation Trust (page 3) – a draft report following the Care Quality Commission (CQC) inspection had been received which is being reviewed by the Trust. NWAS (page 3) – there had been no feedback to date following the CQC inspection. NHS Constitution o Cancer waits 62 days (page 6) – the reported issues have been discussed at previous GB meetings. The standard for 85% of patients to receive first definitive treatment for cancer within 62 days was not met for BwD patients in August. Further work is taking place to improve the figures. o • • • Questions and answers followed. RESOLVED: That the Governing Body noted the contents of the report. 14.087 Governing Body Assurance Framework Update Mr Roger Parr presented the Governing Body Assurance Framework (GBAF); reviewed by the GB on a quarterly basis. The CCG has 5 Corporate Objectives and, to assist with the delivery of the objectives, the CCG manages 10 strategic risks associated with the objectives. This is part of the CCG’s system of internal control and also provides good governance by the GB. The report highlighted the CCG’s Corporate Objectives and indicated those risks being managed. Mr Parr drew members’ attention to one of the risks which had been considered by the QPEC, with a recommendation for the GB to consider. The risk referred to the target for GP workforce capacity, highlighted in section 4, in relation to future plans for Primary Care delivery. It is noted that it was unlikely that the CCG would deliver the target during this period. Mr Parr added that delivery was not currently within the control of the CCG, as the CCG did not commission this area of work. The CCG had been discussing this with NHS England and Health Education England, both locally and across Lancashire but it was unlikely that the CCG would be able to mitigate this risk during this financial year. Questions and answers followed. RESOLVED: That the Governing Body: i. noted the content of the report ii. noted the implications of risk CO4.3 as outlined 14.088 Primary Care Strategy Dr Malcolm Ridgway introduced the Primary Care Strategy. Dr Ridgway stressed the importance of the CCG having a vision and strategy for Primary Care. The document set out an overarching strategic direction to realise the changes required to provide an integrated high quality services model. Page 7 of 10 Mr Peter Sellars outlined the aims of the CCG with regards to Primary Care (General Practice), which as the foundation of care needs to fundamentally change from its current operating arrangements of fragmented services to an integrated high quality services model, having collective responsibility for the health of the population. The report outlined how the CCG would deliver this from the provider aspect, as well as from a commissioning perspective. It was noted that General Practice was under pressure both locally and nationally in terms of the current investment into Primary Care, which has seen a reduction over the last few years. Along with this, General Practices have been requested to do more, e.g. increased GP access and moving some services from a secondary care into a primary care setting. There have also been difficulties relating to the recruitment and retention of GPs. The strategy addressed some of these key issues and set out an operating standard for General Practice. It also outlined what success would look like and how patient benefits could be measured. Questions and answers followed. ACTION: Dr Ridgway noted comments and suggestions from members and agreed to consider their inclusion within the strategy. RESOLVED: That the Governing Body: i. ii. 14.089 received and considered the contents of the paper approved and ratified the strategic direction set out in the paper Co-commissioning Primary Care Update Dr Malcolm Ridgway introduced the co-commissioning update, which provided background to and an update on Co-commissioning Primary Care, in particular the activities and timeframes involved. Mr Peter Sellers outlined the background to the CCG submitting an expression of interest in taking on an increased role in the commissioning of Primary Care Services (General Practice). The CCG submitted an interest in the Category C commissioning of Primary Care (General Practice), which was full delegated authority. Mr Sellars explained the meaning of delegated arrangements, the approvals process and timescales involved. Mr Sellars added that the CCG would need to resubmit its proposal to NHS England by the 5th January 2015, in order to prepare for a commencement date of 1st April 2015. Questions and answers followed. RESOLVED: That the Governing Body received and considered the content of the paper and looked forward to receiving regular reports on progress. 14.090 System Resilience 2014/15 Mrs Debbie Nixon presented the report on System Resilience for 2014/15 which provided an update on Pennine Lancashire plans for operational resilience and capacity planning and to support delivery of the 4 Hour A&E and 18 Weeks RTT targets. It had been agreed by the Governing Bodies across the Pennine Lancashire Health and Social Care Economy that the newly established Chief Executive Officers Steering Page 8 of 10 Group would undertake the role of the System Resilience Group (SRG) and would provide oversight and assurance on shared plans. Mrs Nixon reported that the SRG signed off the initial plans for system resilience in August 2014 to support urgent care and elective activity and agreed jointly how to utilise the non-recurrent resource for the health economy. Mrs Nixon drew members’ attention to the resilience winter funded schemes outlined in the report, some of which were linked to the CCG’s plans for the Better Care Fund. Mrs Nixon added that the plans would be presented to the SRG next week for sign off and then the resource would be allocated to the organisations. Questions and answers followed. RESOLVED: That the Governing Body noted the content of the update. 14.091 External Audit Annual Audit Letter 2013/14 The External Audit Annual Audit Letter 2013/14, which summarised the key findings arising from the work that Grant Thornton had carried out with BwD CCG for the year ended 31st March 2014 was circulated for information. RESOLVED: That the Governing Body noted the content of the letter. 14.092 Governing Body Sub-Committees and Groups’ Summary Mr Iain Fletcher presented the Governing Body Sub-Committees and Groups’ Summary which summarised each Committee Meeting for the Governing Body and identified key decisions or actions and items of particular interest was presented for information. RESOLVED: That the Governing Body noted the content of the report. 14.093 Governing Body and Sub Committees and Groups’ Terms of Reference 14.093.1 Governing Body Mr Iain Fletcher presented the Terms of Reference (ToR) for the GB which had been revised to take into account the number of GPs on the GB 14.093.2 Executive Joint Commissioning Group Mr Iain Fletcher presented the ToR for the Executive Joint Commissioning Group (EJCG) which had been revised following the establishment of the localities within BwD and was linked to the changes in the CCG’s Constitution. RESOLVED: That the Governing Body approved the ToRs for the GB and the EJCG. Mr Fletcher reported that the submission of the revised CCG Constitution would now take place prior to 1st December 2014 and requested approval from the GB for the submission to be signed off by the Chair, following receipt of guidance awaited from NHS England on arrangements to co-commission Primary Care. RESOLVED: That the Governing Body agreed to approve Chair’s Action for the sign off the CCG Constitution prior to its submission to NHS England. Page 9 of 10 14.094 Mental Health Crisis Concordat Update Mrs Debbie Nixon presented the report which provided an overview of the Mental Health Crisis Care Concordat, which BwD CCG was coordinating on behalf of the CCGs across Lancashire. The CCG was working in partnership with Lancashire Constabulary and took part in a successful stakeholder event on 10th October at Lancashire Police Headquarters. Mrs Nixon reported that a comprehensive Action Plan would be in place by 31st March 2015 and work was progressing well. She added that Dr Chris Clayton would sign off the necessary declaration by 31st December 2014, which would commit to CCG to support the developing Action Plan. The Action Plan would be a Lancashire plan but on the footprint of the three Lancashire H&WBBs. The BwD plan would be presented to a future meeting of the BwD H&WBB. RESOLVED: That the Governing Body noted the content of the update. 14.095 Any Other Business No further business was discussed. 14.096 Date and Time of Next Meeting The next meeting will be held on 14th January 2015 at 1 pm, Meeting Rooms 1 & 2 Blackburn Central Library, Town Hall St, Blackburn, BB2 1AG. The Chair thanked everyone for their attendance and input and the meeting closed. EXCLUSION OF THE PRESS AND PUBLIC – ‘That representatives of the press and other members of the public be excluded from the remainder of the meeting having regard to the confidential nature of the business to be transacted, publicity on which would be prejudicial to the public interest’ (Section1(2)Public Bodies(Admission to Meetings)Act 1960) Signed ………………………………………………. Chairman …………………………………… Date Page 10 of 10 CLINICAL COMMISSIONING GROUP (CCG) Item 7.1 Extract from the Minutes of Part 2 of the Governing Body Meeting held on Wednesday 5th November 2014 at 3 pm in the Rooms 1 and 2, Blackburn Central Library, Town Hall Street, Blackburn BB2 1AG PRESENT: Mr Joe Slater Mr Roger Parr Dr Pervez Muzaffar Mr Paul Hinnigan Dr Penny Morris Mrs Debbie Nixon Dr Malcolm Ridgway Dr Adam Black Mrs Anne Asher Chairman (Chair) Chief Finance Officer Executive Member Lay Member - Governance Executive Member Chief Operating Officer Clinical Director for Quality and Effectiveness Executive Member (Part) Lay Member - Nurse Representative IN ATTENDANCE: Mr Iain Fletcher Head of Corporate Business Mrs Pauline Milligan Corporate Support Officer (minutes) A/14 Minutes of Part 2 of the Meeting held on 3rd September 2014 The Minutes of Part 2 of the Meeting held on 3rd September 2014 were considered and accepted as an accurate record. RESOLVED: That the Minutes of Part 2 of the Meeting held on 3rd September 2014 were approved as an accurate record. B/14 B/14.1 Matters Arising/ Action Matrix The following items were noted: Minute C/14 – September – Safeguarding Update Dr Malcolm Ridgway reported that the safeguarding concern raised at the last meeting had been resolved. Dr Ridgway provided a verbal update to the Governing Body (GB) regarding safeguarding issues. Mr Iain Fletcher provided a verbal update on the current position related to Continuing Healthcare (CHC) cases. The GB discussed the difficulties involved in dealing with Deprivation of Liberty Safeguarding (DoLS) assessments, which seemed to be a growing issue nationally. Page 1 of 1 GOVERNING BODY (GB) MEETING - ACTION MATRIX Item 8.1 Action Origin Board Ref 14.083 14.083 14.085 14.088 Action Clinical Chief Officer’s Report It was agreed that developments related to the NHS Five Year Forward Review would be presented to the next meeting of the Governing Body by Mrs Debbie Nixon. Clinical Chief Officer’s Report The Chair agreed to feedback comments related to the communication and engagement of plans for the Pennine Lancashire Mental Health Unit to Lancashire Care NHS Foundation Trust. Contract Performance Report Following a comment from a member of the public Mr Roger Parr agreed to consider a request to include data related to Patient Transport Services in future reports. Primary Care Strategy Dr Malcolm Ridgway noted comments and suggestions from members and agreed to consider their inclusion within the strategy. Owner Due Date Status DN JANUARY 15 JANUARY AGENDA JS JANUARY 15 COMPLETED RP JANUARY 15 COMPLETED MR JANUARY 15 COMPLETED GOVERNING BODY MEETING Date of Meeting Title of Report Governing Body Responsible Officer Summary/Purpose of Report Governing Body Action 14TH JANUARY 2015 Agenda Item No. CLINICAL CHIEF OFFICER’S REPORT 9 Lead DR CHRIS CLAYTON, Clinician CLINICAL CHIEF OFFICER Lead MR IAIN FLETCHER, HEAD OF Manager CORPORATE BUSINESS This report provides an update on national and local issues of interest to Governing Body members not covered elsewhere on the agenda, and provides an indication of where the Clinical Chief Officer’s efforts have been directed since the last meeting. The Governing Body is requested to receive this report and to note the items as detailed. DR CHRIS CLAYTON, CLINICAL CHIEF OFFICER Please indicate the Committee(s)/Group(s) where the paper has been discussed/developed None. Please note the following section must be completed in full N/A Patient and Public (if yes, complete outcome) Engagement Completed N/A (if yes, complete outcome) Equality Analysis Completed N/A Financial Implication(s) Risk(s) Identified N/A CCG Strategic Objectives supported by this paper 1. 2. 3. 4. 5. We will continuously improve the health and well-being of the population of Blackburn with Darwen. We will build successful partnerships which promote collaborative working and integrated service delivery. We will effectively engage patients and the public in decision making. Y We will co-commission and deliver continuous improvement in Primary Care Services and tackle inequalities. We will commission safe and effective services for the population of Blackburn with Darwen with integration at the heart of commissioning. Y CCG High Impact Changes supported by this paper 1. 2. 3. 4. 5. 6. 7. 8. 9. Delivering high quality Primary Care at scale and improving access. Self-Care and Early Intervention. Enhanced and Integrated Primary Care and Better Care Fund. Access to Re-ablement and Intermediate Care. Improved hospital discharge and reduced length of stay. Community based ambulatory care for specific conditions. Access to high quality Urgent and Emergency Care. Scheduled Care. Quality. Report of the Clinical Chief Officer – 14th January 2015 Page 1 of 9 Y Y Y CLINICAL COMMISSIONING GROUP (CCG) GOVERNING BODY MEETING 14TH JANUARY 2015 CLINICAL CHIEF OFFICER’S REPORT 1) Introduction This report provides an update on national and local issues of interest to Governing Body (GB) members not covered elsewhere on the agenda, and also provides an indication of where the Clinical Chief Officer’s (CCO) efforts have been directed since the last meeting. 2) Department of Health 2.1 Female Genital Mutilation NHS England and the Department of Health have issued a joint statement on Female Genital Mutilation. Female Genital Mutilation (FGM) is child abuse and the Department of Health and NHS England are committed to caring for FGM survivors, protecting girls from FGM, and preventing future generations from having to undergo FGM. On 22 July 2014, the UK hosted the first Girl Summit, aimed at mobilising domestic and international efforts to end FGM and child, early and forced marriage (CEFM) within a generation. The Department of Health’s Female Genital Mutilation Prevention Programme, in partnership with NHS England, was launched at the Girl Summit and work on a number of FGM projects is now underway across NHS settings to improve the health response to FGM. Further information via: http://www.england.nhs.uk/2014/12/08/fgm-prevention/ 2.2 Genomes Project Eleven new centres across England have been chosen to deliver the 100,000 Genomes Project. The three year project, launched by the Prime Minister earlier this year, aims to improve diagnosis and treatment for patients with cancer and rare diseases. The initiative involves collecting and decoding 100,000 human genomes – complete sets of people’s genes – that will enable scientists and doctors to understand more about specific conditions. The project has the potential to improve our ability to predict and prevent disease. It may also lead to new and more precise diagnostic tests and the ability to more accurately personalise drugs and other treatments to specific genetic variants. It is anticipated that over 75,000 people will be involved, which will include some patients with life threatening and debilitating disease. After samples are collected, they will be sent securely to Illumina who have been procured by Genomics England to sequence the whole genome and to analyse it. Results will be sent back to the NHS for validation and clinical action. Report of the Clinical Chief Officer – 14th January 2015 Page 2 of 9 The 11 designated Genomic Medicine Centres (GMCs) in this first selection process are based across the country covering areas including Greater Manchester, the North West coast, Oxford, Birmingham and the West Midlands, Southampton, London, Cambridge and the East of England, Exeter and the South West Peninsula, and the North East. Over the lifetime of the project NHS England’s ambition is to secure more than 100 participating NHS trusts. Further information genomics-project via: https://www.gov.uk/government/news/eleven-new-centres-to-lead- 3) NHS England 3.1 Changes to Regional and Area Responsibilities and Senior Appointments On 1st October 2014 NHS England announced plans designed, in part, to streamline and align the functions and structures which support the organisation to work more effectively – both nationally and regionally – to minimise duplication and make more effective use of its resources. A single integrated team for each of the current regions has been developed. Four geographical locations have been identified in each region, taking into account factors such as: numbers of relationships with Clinical Commissioning Groups (CCGs), Trusts, Local Authorities, population size and patients flows. NHS England announced on 28th November the following appointments to the Directors of Commissioning Operations roles: • • • • • • • • • Moira Dumma – Yorkshire and the Humber Graham Urwin – Lancashire and Greater Manchester Clare Duggan – Cheshire and Merseyside Wendy Saviour – North Midlands David Sharp – Central Midlands Andrew Reed – West Midlands Andrew Pike – East Anthony Farnsworth – South West Felicity Cox – South East I am pleased to confirm that Graham Urwin will be coming to Blackburn with Darwen Clinical Commissioning Group (BwDCCG) on 4th February to meet with members of its GB. The following appointments have also been announced for the Lancashire and Greater Manchester region: • • • Raj Patel – Medical Director Trish Bennett – Director of Nursing Ian Currell – Director of Finance 3.2 Friends and Family Test On 1st December the Friends and Family Test (FFT) went live in 8,000 GP practices across England, giving up to a million patients a day the opportunity to have a say about their care and treatment. The FFT aims to drive service improvement in local healthcare by providing people with the opportunity to feedback on their experience. Report of the Clinical Chief Officer – 14th January 2015 Page 3 of 9 Further information via: http://www.england.nhs.uk/ourwork/pe/fft/ 3.3 Winter Resilience NHS England produces a summary which offers an overview of the system and pulls together information on waiting times in Accident and Emergency (A&E) Departments, ambulance response times, daily situation reports from the NHS, and information on flu rates. The Weekly A&E Attendances and Emergency Admissions collection collects the total number of attendances in the week for all A&E types, including Minor Injury Units and Walk-in Centres, and of these, the number discharged, admitted or transferred within four hours of arrival. Also included are the number of Emergency Admissions, and any waits of over four hours for admission following decision to admit. Data are shown at provider organisation level, from NHS Trusts, NHS Foundation Trusts and Independent Sector Organisations. Data for this collection is available back to November 2010. The weekly A&E figures for the weeks ending 21st December and 28th December 2014, which is a particularly busy time for services have been published. The figures show that in the three months to the end of December more than nine out of ten A&E patients in England continued to be seen and treated in under four hours – the best measured performance of any major western country. In the immediate run up to Christmas the NHS treated 446,500 A&E attendees, up 38,000 on the same week last year. There were 112,600 emergency admissions – the highest number in a single week since figures began to be published in 2010. A similar demand was faced over Christmas itself. In the week ending 28th December, A&E attendances were up more than 31,000 on the same period last year, meaning that the NHS successfully treated more patients in under four hours than ever before. 3.3.1 Pennine Lancashire There is a great deal of pressure on the system “nationally” and locally and across services - GPs and other services are all busy; Social Services referrals are very high. All Health and Social care services are working together actively and are under increasing pressure – all staff are working extremely hard to make sure that patients receive safe, high quality care. The vast majority of patients attending A&E are being seen within target time period. Despite talk of lengthy waiting times, 84% (92% nationally) of people are being seen within the target. Further information via: http://www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-and-activity/ 3.4 Coalition for Collaborative Care A major new alliance committed to improving care and support for people with long-term conditions was launched on 21st November. The Coalition for Collaborative Care (C4CC) has people with long-term health conditions at the heart of its powerful alliance and brings together some of the sector’s most influential national groups and organisations. Report of the Clinical Chief Officer – 14th January 2015 Page 4 of 9 With more than 15 million people in the UK living with a long-term condition, the Coalition will champion a system-wide transformation in how they receive and use care and support. This innovative new partnership will focus on re-framing the relationship between a person with long-term health conditions and the professionals supporting them. This allows the expertise of both to be used most effectively to help the person plan to manage their condition and maximise their well-being. It will draw strongly on the House of Care developed by the Year of Care Partnerships which highlights what is required to achieve person-centred coordinated care. There is good evidence to suggest that engaging with people with long-term conditions to codesign their care, leads to better outcomes and more successful independent living. C4CC aims to ensure that professionals and people have the right support, knowledge, skills, power and confidence to achieve this. The Coalition will also put a strong emphasis on a much more holistic approach in which there is less focus on a person’s condition in isolation and more on the full spectrum of support that is required to enable people to be included in and play active, valued roles within their own communities – an approach developed by Nesta in its People Powered Health programme and often called ‘More than Medicine’. Further information via: http://www.england.nhs.uk/2014/11/21/c4cc/ 4) Blackburn with Darwen Clinical Commissioning Group 4.1 Lancashire Care NHS Foundation Trust (LCFT) The Trust has been informed that planning permission for the proposed new Pennine Lancashire Mental Health Unit inpatient facility on the land immediately adjacent to the Royal Blackburn Hospital site, which will provide 72 beds for adults over the age of 18, has been granted by Blackburn with Darwen (BwD) Borough Council. 4.2 East Lancashire Hospitals NHS Trust (ELHT) See under Item 3.3 – Winter Resilience. 4.3 Midlands and Lancashire Commissioning Support Unit Following a restructure, the Commissioning Support Unit (CSU) has announced the following appointments in its leadership team to support Derek Kitchen, Managing Director. • • • • • • • • Peter Spilsbury - Director of Strategy Unit Carl Usher - Director of Finance and Commerce Deb Thwaites – Director of Business Improvement Tony Matthews – Director of Operations Sarah Sheppard – Director of People Linda Riley – Director of Clinical Services Stephanie Belgeonne and Lynda Scott – Communications and Engagement Service Chris Knight – Business Executive Lead 4.4 Care.data The CCG is a pathfinder for the care.data initiative and is working with NHS England. Report of the Clinical Chief Officer – 14th January 2015 Page 5 of 9 The CCG will engage with all relevant stakeholders, including patient groups, in launching the initiative. BwD Healthwatch is also involved and will inform the learning from the pilot stages. 4.5 Better Care Fund Following the submission of further evidence to move its plans for the Better Care Fund (BCF) to a fully approved status, the CCG is pleased to have been informed by NHS England that, following the subsequent Nationally Consistent Assurance Review (NCAR) process, its plans have been classified as ‘Approved’. NHS England stated that it was clear that the CCG’s team and partners have worked very hard over the last year to develop its plan to improve people’s care and that the plan was clear and ambitious. NHS England supported BwD’s ambitions and stated it was in a strong position to deliver the changes outlined in the plan; that it was confident that there were no areas of high risk and that BwD should progress with implementation. 5) Blackburn with Darwen Health and Well-being Board 5.1 Joint Health and Well-being Strategy The Blackburn with Darwen Joint Health and Well-being Strategy has been refreshed and it is now structured around three life stages: • • • Start Well Live Well Age Well It is intended that this will allow for the work to be overseen by the Children’s Partnership Board, the local Prosperous Group of the Local Strategic Partnership and the 50+ Partnership respectively. These bodies are aware of the need to allow for overlap as people make the transition from child to adult and from working age to retirement. The next steps will be: • • • • • • Continue 1:1 and group discussions with key stakeholders to refine the priorities further and clarify relationship with other partnership priorities and programmes of work Stakeholder workshops to agree a small number of evidence based actions for the achievement of each priority. These will be led by the thematic delivery groups (Children’s Partnership Board, Prosperous Group and 50+ Partnership) Agree outcomes and associated proxy measures that will demonstrate progress toward achieving outcomes Agree a performance reporting process that provides the Board with sufficient assurance of progress and alerts the Board to areas requiring corrective action. This will be integrated with other performance reporting processes so far as is possible Finalise delivery structures and reporting arrangements and update as necessary including role of Prosperous Group ‘Sense check’ with thematic and other groups/partners affiliated to the Health and Wellbeing Board (HWBB). 5.2 Regional Voices This annual ‘Supporting Influence on HWBBs’ survey asks the voluntary, community and social enterprise (VCSE) sector about engagement with HWBBs – what is working well, what could work better and what support would help. The aim of the survey is to capture how VCSE engagement with HWBBs is changing over time. Report of the Clinical Chief Officer – 14th January 2015 Page 6 of 9 The survey is aimed at: • • • Voluntary sector representatives on HWBBs Healthwatch representatives on HWBBs The wider voluntary, community and social enterprise sector It asks about routes into the H&WBB, how the VCSE sector is able to influence the Joint Strategic Needs Assessment, the Joint Health and Well-being Strategy and local commissioning. It is hoped to capture how engagement with the Boards is changing over time. It also includes a new question, looking at HWB use of local Compacts. The closing date for this survey is 23 January 2015. Further information via: https://www.surveymonkey.com/s/HWBengagementsurvey3?utm_medium=email&utm_source=T he+King%27s+Fund+newsletters&utm_campaign=5071556_HMP+2014-1202&dm_i=21A8,30P8K,HPWAEQ,AV2DS,1 6) Good News 6.1 North West Towards Excellence The Finance Skills Development Network has announced that Level 1 Accreditation has been awarded to the Lancashire CCGs. This is an excellent achievement which not only demonstrates continuous improvement and development of the finance function within the Lancashire organisations but also a culture of collaborative working. 6.2 Health Business Awards The Health Business Awards has established a reputation for showcasing the success stories in the health sector. The Awards recognise and celebrate the significant contributions made each year by organisations and individuals that work inside and alongside the NHS. The NHS Collaboration Award is presented to the NHS Trust which has worked with other public/private sector organisations, such as local government, police, fire, charities, schools etc. to engage the local community in preventative campaigns. I am pleased to announce that an innovative project to reduce the demands on hospital and police staff in A&E at the Royal Blackburn Hospital (RBH) has scooped the award for collaboration in 2014. The scheme involves two highly trained and extensively skilled Police Officers placed within the A&E department at the RBH and is funded by the CCG commissioners across East Lancashire (in Pennine Lancashire). The A&E scheme went up against stiff opposition and won due to the partnership and team work between Lancashire Constabulary and the NHS in Pennine Lancashire – involving BwDCCG, East Lancashire CCG, ELHT and LCFT. The scheme consists of a Pennine Lancashire Hospital Early Action Team which is based at the hospital to provide a more co-ordinated and integrated police support role within A&E. The scheme seeks to support individuals who visit A&E in a distressed state as the result of alcohol Report of the Clinical Chief Officer – 14th January 2015 Page 7 of 9 and substance misuse or mental health problems. The aim is to manage these vulnerable individuals where they live using community based resources. The officers have worked with hospital staff to identify and support individuals who attend A&E as a result of challenging behaviour, alcohol, substance misuse, a mental health problem, housing issues and loneliness. The organisations involved in the scheme established it to help reduce pressure on A&E as well as actively support those patients affected within the community. The scheme began in April this year, and is now fully operational. I am delighted that this award recognises the integrated work and collaboration between all of our organisations. Patients and the public tell us that health and other services could be better joined up and this is a perfect example where organisations have worked collectively to achieve this in A&E. Patients should be reassured that we are working hard together to achieve the best outcomes and services for them. 6.3 Excellence in Diversity Awards I am pleased to announce that the CCG has been nominated for the Diverse Company Award: Public in the Excellence in Diversity Awards 2015. The Excellence in Diversity Awards is the only awards ceremony that rewards UK organisations for harnessing a truly diverse workforce, thus recognising the significant efforts of companies nationwide that excel in their commitment to diversity and inclusion. The Excellence in Diversity Awards also focus on leading diversity champions, significant role models and extraordinary employees that have displayed motivation, innovation and commitment to the equality agenda. Shortlisted nominees will be chosen following the close of nominations and will be invited to attend the ceremony in May 2015. 6.4 Crisis Care Concordat BwDCCG, as the Lead Commissioner for the mental health contract, submitted a bid on behalf of all CCGs. This bid was for additional monies linked to the Crisis Care Concordat. The bid was successful and an additional £868k has been allocated to a number of schemes to allow an increase in existing unscheduled care services or new pilot schemes to be tested across Lancashire whilst ongoing redesign of the services is undertaken. The intended outcome is that the schemes are embedded as part of the overall unscheduled care/ service and is within current resources following the redesign which is a Lancashire wide commissioning intention. 7) Meetings Members may be interested to note the following meetings and events which have taken place during the course of the last two months. 4 November 5 November 6 November 6 November North Tripartite Autumn Event CCG Leaders meeting with Jeremy Hunt, Secretary of State for Health CCG Executive Team Development Session Practice Visit to Cornerstone Practice Report of the Clinical Chief Officer – 14th January 2015 Page 8 of 9 7 November 10 November 11 November 12 November 13 November 14 November 19 November 20 November 24 November 26 November 26 November 27 November 27 November 2 December 3 December 3 December 3 December 4 December 4 December 8 December 9 December 10 December 17 December 18 December Residents Meeting with Jack Straw, MP (Shadsworth with Whitebirk/Audley) Practice Visit to Little Harwood Health Centre Practice Visit to The Montague Practice Pennine Lancashire Chief Executives Steering Group Local Medical Committee Residents Meeting with Jack Straw, MP (Higher Croft) Health Service Journal Awards Protected Learning Time Event, Urgent Care in Children and the Elderly Executive Joint Commissioning Group CCG Staff Meeting Practice Visit to The Family Practice Lancashire CCG Network Lancashire Leadership Forum Blackburn with Darwen GP Development Session Governing Body Development Session Governing Body Development and Discussion Meeting Pennine Lancashire Clinical Transformation Board Practice Visit to Waterside Surgery Practice Visit to Umar Medical Centre Practice Visit to Brownhill Surgery Practice Visit to Roe Lee Surgery Pennine Lancashire Chief Executives Steering Group Clinical and Management Executive Team Practice Visit to Dr Hirst, Darwen Health Centre 8) Recommendation The Governing Body is requested to receive this report and to note the items as detailed. Dr. Chris Clayton Clinical Chief Officer 5th January 2015 Report of the Clinical Chief Officer – 14th January 2015 Page 9 of 9 GOVERNING BODY MEETING Date of Meeting Title of Report Governing Body Responsible Officer 14TH JANUARY 2015 Agenda Item No. CHIEF FINANCE OFFICER’S REPORT 10 Lead Clinician Lead MRS LINDA RING, SENIOR Manager FINANCE MANAGER The current revenue position is on plan to deliver the planned Summary/Purpose of year end surplus of £2,307k. Year to date (YTD) the Clinical Report Commissioning Group (CCG) is reporting a cumulative breakeven position. A breakeven position is forecast at year end. The current forecast is based on best estimates of future expenditure. Increasing acute activity and Continuing Healthcare pressures within the health system remain a factor. It is recommended that the CCG Governing Body note the Governing Body contents of this financial summary and the overall position of the Action CCG at the end of November 2014, noting the risks and detailed appendices supporting this narrative. Please indicate the Committee(s)/Group(s) where the paper has been discussed/developed N/A MR ROGER PARR, CHIEF FINANCE OFFICER Please note the following section must be completed in full N/A Result Patient and Public Engagement Completed N/A Result Equality Analysis Completed N/A Financial Implication(s) Yes Risk(s) Identified CCG Strategic Objectives supported by this paper 1. 2. 3. 4. 5. We will continuously improve the health and well-being of the population of Blackburn with Darwen. We will build successful partnerships which promote collaborative working and integrated service delivery. We will effectively engage patients and the public in decision making. We will co-commission and deliver continuous improvement in Primary Care Services and tackle inequalities. We will commission safe and effective services for the population of Blackburn with Darwen with integration at the heart of commissioning. Y Y Y Y Y CCG High Impact Changes supported by this paper 1. 2. 3. 4. 5. 6. 7. 8. 9. Delivering high quality Primary Care at scale and improving access. Self-Care and Early Intervention. Enhanced and Integrated Primary Care and Better Care Fund. Access to Re-ablement and Intermediate Care. Improved hospital discharge and reduced length of stay. Community based ambulatory care for specific conditions. Access to high quality Urgent and Emergency Care. Scheduled Care. Quality. Y Y Y Y Y Y Y Y Y Executive Financial Summary Month 8 – Period Ending 30th November 2014 Funds Available Budget £000 139,324 Year to Date Actual £000 139,324 109,865 20,920 4,775 2,228 1,536 112,303 20,800 4,685 0 1,536 Variance £000 0 Budget £000 208,225 Full year forecast Actual £000 208,225 (2,438) 120 90 2,228 0 164,926 31,384 7,380 2,228 2,307 167,523 31,224 7,171 0 2,307 Variance £000 0 Commissioning Primary Care Corporate Reserves Balance (2,597) 160 209 2,228 0 Summary Financial Position ‐ The current revenue position is on plan to deliver the planned year end surplus of £2,307k. Year to date (YTD) the CCG is reporting a cumulative breakeven position. A breakeven position is forecast at year end. The current forecast is based on best estimates of future expenditure. Increasing acute activity and CHC pressures within the health system remain a factor. Commissioned Services RISKS • Healthcare Commissioning from providers is reporting a YTD overspend • Acute activity levels continue to be a key factor in 2014‐15. of £2,438k with a year‐end forecast overspend of £2,597k. The Schemes are in place to reduce non elective admissions with our overspending is mainly due to pressures in A&E, elective inpatients, main provider. critical care and radiology. The forecast is based on month 7 activity. • Continuing health care and complex packages continues to be a • Primary Care Services are reporting a YTD underspend of £120k and key risk. Data has been received for month 7 and this is being forecast underspend of £160k. Prescribing is reporting a small verified. This area of spend will be closely monitored in 2014‐15. overspend at November offset by savings reported on enhanced • Prescribing expenditure is volatile and is monitored closely by services and other primary care commissioning. Prescribing is based the Medicines Management Team. on actual spend to September with forecast spend for October and November. QIPP • Corporate Services are reporting a YTD underspend of £90k and • 67% of the QIPP target has been achieved at month 8 which is in forecasting a year end underspend of £209k mainly due to the CCG plan to meet a full year target of £4m. operating within its running cost allowance. Capital • The overspend in commissioning is covered by underspends in primary care, corporate services and reserves. • The CCG is planning Primary Care IT capital expenditure of £181k on infrastructure upgrade. YTD expenditure of £118k has been incurred. Recommendation ‐ It is recommended that the CCG Governing Body note the contents of this financial summary and the overall position of the CCG at the end of November 2014, noting the risks and detailed appendices supporting this narrative. NHS Blackburn with Darwen CCG APPENDIX A Summary Governing Body Report ‐ November 2014 Budget to Date £000 Expenditure to Date £000 Variance to Date £000 Annual Budget £000 Annual Forecast Variance £000 Annual Forecast £000 Revenue Resource Limit Confirmed (139,324) (139,324) 0 (208,225) (208,225) 0 0 0 0 0 0 0 (139,324) (139,324) 0 (208,225) (208,225) 0 (2,437) Anticipated Total Revenue Resource Limit Expenditure Commissioning (Page 2) 130,785 133,103 (2,318) 196,310 198,747 Corporate (Page 4) 2,326 2,298 28 3,409 3,400 9 Reserves (Page 4) 2,228 0 2,228 2,228 0 2,228 135,339 135,401 (62) 201,947 202,147 (200) Healthcare Sub Total Running Costs (Page 4) Total Expenditure Surplus/(Deficit) Better Payment Practice Code NHS Non NHS 2,449 2,387 62 3,971 3,771 200 137,788 137,788 0 205,918 205,918 0 1,536 1,536 0 2,307 2,307 0 YTD Value (%) YTD Volume (%) FOT Value (%) FOT Volume (%) Target (%) 100.0 98.5 100.0 98.5 95.0 98.1 99.2 98.1 99.2 95.0 Page 1 NHS Blackburn with Darwen CCG Healthcare Commissioning Report ‐ November 2014 Budget to Date Expenditure to Date Variance to Date £000 £000 £000 Annual Budget £000 Annual Forecast £000 Acute Services NHS contracts (includes Ambulance Services) 74,482 75,725 (1,243) 111,723 113,488 3,241 3,885 (644) 4,862 5,175 NHS Contract Exclusions / Cost per Case 412 319 93 618 434 Non Contract Activity 491 733 (242) 736 749 Non NHS Providers Other 0 0 0 0 0 78,626 80,662 (2,036) 117,939 119,846 10,541 10,541 0 15,762 15,762 466 440 26 651 611 NHS Contract Exclusions / Cost per Case 92 83 9 107 103 Non Contract Activity 22 3 19 33 33 Sub Total Acute Contracts Mental Health Services NHS contracts Non NHS Providers Other (221) (217) (4) (221) (217) 10,900 10,850 50 16,332 16,292 NHS contracts 9,537 9,537 0 14,305 14,305 Non NHS Providers 1,358 1,403 (45) 1,947 1,718 116 105 11 174 150 0 0 0 0 0 701 701 0 1,049 1,049 Sub Total Mental Health Services Community Health Services NHS Contract Exclusions / Cost per Case Non Contract Activity Hospices Other Sub Total Community Services Total Healthcare Contracts 407 16 391 1,229 1,230 12,119 11,762 357 18,704 18,452 101,645 103,274 (1,629) 152,975 154,590 4,570 5,326 (756) 6,466 7,450 320 389 (69) 480 502 4,890 5,715 (825) 6,946 7,952 26,463 Continuing Care Services Continuing Care Free Nursing Care Sub Total Continuing Care Services Primary Care services Prescribing 17,635 17,641 (6) 26,453 Enhanced Services 432 353 79 648 528 Out of Hours 757 757 0 1,135 1,135 1,712 1,684 28 2,564 2,558 384 365 19 584 540 20,920 20,800 120 31,384 31,224 77 61 16 125 101 Commissioning Other Sub‐total Primary Care services Other Programme Services Other Non Acute Complex Cases & Individual Funding Requests Sub Total Other Programme Services Surplus/(Deficit) 3,253 3,253 0 4,880 4,880 3,330 3,314 16 5,005 4,981 130,785 133,103 (2,318) 196,310 198,747 Page 2 APPENDIX B Annual Forecast Variance £000 (1,765) (313) 184 (13) 0 (1,907) 0 40 4 0 (4) 40 0 229 24 0 0 (1) 252 (1,615) (984) (22) (1,006) (10) 120 0 6 44 160 24 0 24 (2,437) Page 3 NHS Blackburn with Darwen CCG APPENDIX C Main Healthcare Contracts ‐ November 2014 Expenditure to Date £000 Budget to Date £000 Variance to Date £000 Annual Budget £000 Annual Forecast £000 Annual Forecast Variance £000 Acute Contracts Main Provider East Lancashire Hospitals NHS Trust 64,390 64,963 (573) 96,586 97,445 (859) 3,092 3,415 (323) 4,638 5,022 (384) 321 349 (28) 481 524 (43) 54 103 (49) 81 155 (74) Other Lancashire Providers Lancashire Teaching Hospitals NHS FT Blackpool Fylde & Wyre Hospitals NHS FT University Hospitals Morecambe Bay NHS FT North West Ambulance Service NHS Trust (Block) 4,465 4,465 0 6,697 6,697 0 Sub Total Other Lancashire Providers 7,932 8,332 (400) 11,897 12,398 (501) University Hospital South Manchester NHS FT 269 328 (59) 404 492 (88) Salford Royal NHS FT 242 170 72 362 255 107 Royal Bolton Hospitals NHS FT 173 226 (53) 259 339 (80) Wrightington, Wigan & Leigh NHS FT 351 444 (93) 526 666 (140) Central Manchester University Hospital NHS FT 870 969 (99) 1,306 1,454 (148) Greater Manchester Providers Pennine Acute NHS Trust Sub Total Greater Manchester Providers 120 107 13 180 160 20 2,025 2,244 (219) 3,037 3,366 (329) Merseyside providers Royal Liverpool & Broadgreen NHS Trust 136 186 (50) 203 280 (77) Sub Total Merseyside Providers 136 186 (50) 203 280 (77) 2,564 3,254 (690) 3,846 4,230 (384) 211 164 47 316 245 71 2,775 3,418 (643) 4,162 4,475 (313) 77,258 79,143 (1,885) 115,885 117,964 (2,079) 10,036 10,036 0 15,053 15,053 0 482 482 0 674 674 0 21 21 0 32 32 0 10,539 10,539 0 15,759 15,759 0 Lancashire Care NHS FT (Block) 9,537 9,537 0 14,305 14,305 0 Total Community Health Contracts 9,537 9,537 0 14,305 14,305 0 97,334 99,219 (1,885) 145,949 148,028 (2,079) Independent Sector Contracts BMI Healthcare (Beardwood, Beaumont, Gisburne) Ramsay Sub Total Total Acute Contracts Mental Health Contracts Lancashire Care NHS FT (Block) Calderstones Partnership NHS FT (Block) Greater Manchester West NHS FT Total Mental Health Contracts Community Health Contracts Surplus/(Deficit) Page 4 NHS Blackburn with Darwen CCG APPENDIX D Non Healthcare Commissioning Report ‐ November 2014 Budget to Date £000 Expenditure to Date Variance to Date £000 £000 Annual Budget £000 Annual Forecast Variance £000 Annual Forecast £000 Other Corporate Costs (Non‐Running Costs) CSU re‐charge 397 382 15 566 566 1,439 1,439 0 2,158 2,158 0 490 477 13 685 676 9 2,326 2,298 28 3,409 3,400 9 Reserves 2,228 0 2,228 2,228 0 2,228 Sub Total Reserves 2,228 0 2,228 2,228 0 2,228 25 NHS Property Services re‐charge Other Sub Total Corporate Costs 0 Plan requirements & reserves Running Costs CCG Pay 1,052 1,046 6 1,585 1,560 CSU re‐charge 909 909 0 1,364 1,364 0 NHS Property Services re‐charge 108 109 (1) 162 162 0 Other 380 323 57 547 479 68 0 0 0 313 206 107 Sub Total Running Costs 2,449 2,387 62 3,971 3,771 200 Surplus/(Deficit) 7,003 4,685 2,318 9,608 7,171 2,437 Running Costs Reserve Page 5 NHS Blackburn with Darwen CCG APPENDIX E Statement of Financial Position ‐ November 2014 Statement of Financial Position November £000 Non Current Assets Property, Plant, Equipment 0 Total Non Current Assets 0 Current Assets Trade and Other Receivables Financial Assets Current Assets Cash and Bank 467 0 0 468 Total Current Assets 935 Total Assets 935 Current Liabilities Trade and Other Payables Other Liabilities Provisions Borrowings (11,137) (42) 0 0 Total Current Liabilities (11,179) Total Assets less Current Liabilities (10,244) Non Current Liabilities Trade and Other Payables Provisions Borrowings Other Liabilities 0 0 0 0 Total Non Current Liabilities 0 Total Assets Employed (10,244) Financed By General Fund Revaluation Reserve Donated Asset Reserve Government Grant Reserve Other Reserves (10,244) 0 0 0 0 Total Equity (10,244) Page 6 CLINICAL COMMISSIONING GROUP (CCG) GOVERNING BODY MEETING Date of Meeting Title of Report Governing Body Responsible Officer Summary/Purpose of Report 14th JANUARY 2015 Agenda Item No. CONTRACT PERFORMANCE REPORT MR ROGER PARR, CHIEF FINANCE OFFFICER 11 Lead Clinician Lead Manager MRS ELAINE BUCKLEY, CONTRACT MANAGEMENT LOCALITY LEAD This report provides the Clinical Commissioning Group (CCG) Governing Body with an update on the activity performance of the major commissioned services of the organisation. The report relies upon aggregated anonymised data supplied by the Midlands and Lancashire Commissioning Support Unit. Governing Body Action The Governing Body is requested to note the content of the report and the supporting appendices. Please indicate the Committee(s)/Group(s) where the paper has been discussed/developed Please note the following section must be completed in full Patient and Public Result Engagement Completed Equality Analysis Result Completed Financial Implication(s) Nil Risk(s) Identified N/A CCG Strategic Objectives supported by this paper 1. 2. 3. 4. 5. We will continuously improve the health and well-being of the population of Blackburn with Darwen. We will build successful partnerships which promote collaborative working and integrated service delivery. We will effectively engage patients and the public in decision making. We will co-commission and deliver continuous improvement in Primary Care Services and tackle inequalities. We will commission safe and effective services for the population of Blackburn with Darwen with integration at the heart of commissioning. Y Y N/A Y Y CCG High Impact Changes supported by this paper 1. 2. 3. 4. 5. 6. 7. 8. 9. Delivering high quality Primary Care at scale and improving access. Self-Care and Early Intervention. Enhanced and Integrated Primary Care and Better Care Fund. Access to Re-ablement and Intermediate Care. Improved hospital discharge and reduced length of stay. Community based ambulatory care for specific conditions. Access to high quality Urgent and Emergency Care. Scheduled Care. Quality. 1 | P a g e N/A Y Y N/A Y Y Y Y Y CLINICAL COMMISSIONING GROUP (CCG) GOVERNING BODY MEETING 14 JANUARY 2015 CONTRACT PERFORMANCE REPORT MONTH 7 1. Introduction 1.1 This report provides the Clinical Commissioning Group (CCG) Governing Body with an update on the activity performance of the major commissioned services of the organisation. The report relies upon aggregated anonymised data supplied by the Midlands and Lancashire Commissioning Support Unit (MLCSU). 2. Lancashire Care Foundation Trust - Mental Health 2.1 The CCG as lead commissioner for mental health services from Lancashire Care NHS Foundation Trust (LCFT) agreed a reporting pause for Quarter 3 in contract year 201415, in order to support the assurance of the top 50 indicators provided by LCFT. Due to this agreement there will be no data received from LCFT other than agreed exceptions to the pause including Out of Area Treatments (OATS), Improving Access to Psychological Therapies (IAPT) and the Memory Assessment Service (MAS). Full reporting will resume at month 10. 2.2 The quarter 3 data will be supplied in January 2015 in line with agreed timescales and will be broken down monthly. Monthly updates on progress for the Top 50 indicators will be shared with Blackburn with Darwen CCG (BwD CCG). 2.3 The tables below contain data for BwD CCG for Admissions and Occupied Bed Days incurred out of the area per month. OATS Admissions Bed Type Functional PICU CCG NHS Blackburn with Darwen CCG NHS Blackburn with Darwen CCG Grand Total OATS Occupied Bed Days Bed Type Functional PICU Grand Total 2 | P a g e CCG NHS Blackburn with Darwen CCG NHS Blackburn with Darwen CCG Apr‐ 14 May‐ 14 Jun‐ 14 Jul‐ 14 Aug‐ 14 Sep‐ 14 Oct‐ 14 YTD 2 4 6 2 0 0 0 14 0 0 1 0 0 0 3 4 2 4 7 2 0 0 3 18 Apr‐ 14 May‐ 14 Jun‐ 14 Jul‐ 14 Aug‐ 14 Sep‐ 14 Oct‐ 14 YTD 38 67 104 38 0 0 0 247 60 37 28 1 0 0 23 149 98 104 132 39 0 0 23 396 2.4 BwD CCG has a monthly target of 246 patients entering psychological treatment to meet the 15% prevalence target. The table below shows the number of patients entered into psychological therapies with LCFT and the Lancashire Women’s Centre for the CCG. In month 7, 295 patients entered into treatment against a target of 246 (+49, +19.9%). Should this performance continue during the final quarter of the year, the Q4 target would be exceeded by 20%. This target continues to be closely monitored and a further update will be given in the month 8 report. Monthly Variance Compared to Q4 Target IAPT Performance 2014‐ 15 Target by Q4 14‐15 Patients Entered Treatment Variance % Variance 2.5 Apr May Jun Jul Aug Sep Oct Total 246 246 246 246 246 246 246 1722 177 230 309 317 183 250 295 1761 ‐69 ‐28.0% ‐16 ‐6.5% +63 +25.6% +71 +28.9% ‐63 ‐25.6% +4 ‐1.6% +49 +19.9% +39 +2.3% The referral number in October exceeded the target for the second month running. BwD CCG received 415 referrals against a target of 295. Self-referrals continue to be promoted in all areas via GPs, primary care professionals, third sector and in the community. Historically, the post-Christmas period yields considerable increases in referral rates, and as such, the Trust are confident in meeting the year-end target, which will be measured via quarter 4, uploads of activity to the National IAPT System. 3. Referrals to Secondary care 3.1 The referrals for treatment to the CCG’s main provider, East Lancashire Hospitals NHS Trust (ELHT) are monitored monthly. From the table below it can be seen that month 7 is showing a slight increase in activity compared to the same period last year. The referral activity measured on an average working day shows an increase from the previous year (3.3%). Referral Type GP Other Excluded Total Average / working day 2014‐15 16,737 5445 4951 27,133 182.1 2013‐14 16,388 4930 5117 26,435 176.2 Variance 2.1% 10.4% ‐3.2% 2.6% 3.3% Month 7 Year‐on‐Year Comparison: October 2014 3.2 At specialty level, ENT referrals (GP) continue to show an increase at month 7, +177 (12.9%). ELHT have reported that a higher number of 2 week rule referrals for suspected cancer are coming into the service, (monthly average 2013/14 = 24, monthly average 2014/15 = 33). This accounts for at least a third of the variance. Routine referrals from GP’s have also increased from last year. 3.3 Ophthalmology (GP) referrals continue to be under plan, -485 (-21.5%) when compared YTD, with the previous year. The general trend across Lancashire for Ophthalmology shows referrals across the eight CCG’s has decreased compared to last year. ELHT have advised that, due to staffing issues, they have reduced the number of Choose and 3 | P a g e Book slots for this service. The Trust is currently looking at service redesign of this specialty. 3.4 Appendix 1 contains the details of GP referrals to ELHT by specialty. The Specialist Advice Service has now been renamed Advice and Guidance to ensure consistency of approach from a system and familiarity purpose for GP’s. The scheme has been implemented from 1st December 2014 across all 3 specialities (Gynaecology, Haematology and Urology). Weekly teleconferences are taking place between commissioners and ELHT to monitor the progress of the scheme and ensure that it meets agreed timescales and deadlines. The CCG are awaiting activity figures from ELHT in relation to advice requests. 4. Acute Contract Performance – East Lancashire Hospitals Trust 4.1 There has been an increase in the Elective care over trade at month 7. ELHT have adjusted the activity profile for some specialties without prior agreement from the CCG. As a result, the contract monitoring performance summary for Elective will not be available until the month 8 report. Point of delivery A and E (inc Minor Injuries Unit) Non Elective inc. ‘Non Elective Non Emergency’ Outpatients (inc procedures) Financial Variance £k % +193 +7% +304 +2% +36 +0.5% Activity Variance % +1326 +4% +59 +0.5% +1307 +2% 4.2 The non-elective (including non-elective non-emergency) activity, shows performance is above plan +59 (+0.5%), +£304k (+2%). Non-elective performance is also above plan +92 (+0.9%), +£278K (+1.9%). However, non-elective non-emergency activity is below plan for the CCG -33 (-2.0%), although finance is above plan at +£26K (+1.0%). The under performance in non-elective non-emergency care is mostly due to Midwifery, as more patients are being coded intermediate or intensive than standard, indicating more complex pregnancies. 4.3 For ordinary non-elective care, medical specialties are over performing against planned cost levels by +£131K (+2%), although below plan in terms of activity [-72 spells, -1.0%]. Paediatrics is over performing against plan, +£183K (+14%), [+187 spells, +10%]. The Trust has previously advised that overall ELHT are experiencing an increase in NonElective Admissions for paediatrics. The number of admissions to the Children’s Outpatient Assessment Unit (COAU) is increasing year on year including those admitted through Primary Care. 4.4 The graph on page 6 illustrates the pattern of activity beginning in April 2012 for nonelective admissions (NEL). This is the activity at ELHT (which is 96% of BwD CCGs nonelective activity). 4 | P a g e 4.5 This gra aph shows that t perform mance was s close to plan in Octoober (1,532 spells verssus plan 1,530). Year to date overr performan nce now sho ows +92 speells (+0.9%). 4.6 Overall, NEL Adm missions are e currently y slightly higher than last year (2013-14).. A y levels see en in Surgic cal Specialtties (-38, -33.2%) has been b offset by reduction in activity es in Medical Specia alties, ENT T, Gynaeco ology, Rheuumatology, Trauma and a increase Orthopaedics and in n particularr Paediatrics s (+85, +4.4 4%). nce – Othe er Acute Prroviders 5. ELHT Contractt Performan 5.1 At BMI Beardwood d, the contrract is overr performing g by £555kk (+27.2%). The electtive over pe erformance is mainly attributable e to Traum ma and Orrthopaedics s (+96 spe ells, +39.1%)) and General Surgeryy (+78 spells, +28.8%). In both sppecialties, th here has be een an incre ease in the e number o of GP practtices referring into BM MI (5 practices last ye ear compare ed to 11 YT TD). Outpatiient appointments are over plan i n addition to t admissio ons, which in ndicates tha at the activitty is across s the full pa athway and driven by an a increase e in referralss. 5.2 At Lanca ashire Teac ching Hospiitals, there is over perfformance inn elective ac ctivity +£15 55k, (+18.0% %). The overr performan nce is mainly attributab ble to Traum ma and Orth hopaedics and a Gynaeco ological Oncology. 6. ELHT Waiting Lists L 6.1 5 | P 5 age The inpatient and daycase w waiting list by specialty for the CCG’s ma ain providerr is detailed in appendix 4. The tottal size of the waiting list has incrreased by 166 1 patientss in ory 0 to 6 weeks (this iss showing an a increase e of October with the main increasse in catego mparison to o Septembe er). Howeve er, the waitiing list for 6 to 13 wee eks 200 patients in com eptember. This T indicates that addditional activ vity has takken has deccreased by 21 from Se place in n Septemb ber followin ng reduced d activity during d the August ho oliday period. Ophthalmology remains a concern, accounting for 63% of the overall waiting list growth, and is experiencing growth across all waiting time categories. 6.2 The CCG will receive Referral to Treatment (RTT) funding that has been allocated to support achievement of the 18 week RTT target. A contract variation has been agreed for the additional activity and weekly monitoring reports are being provided by the Trust. 7. 36+ week waiters 8. 7.1 The CCG has 8 patients on an incomplete patient pathway waiting over 36 weeks. These are as follows; 2 at Central Manchester University Hospitals; 1 at Lancashire Teaching Hospitals; 3 at East Lancashire Hospitals and 2 at the University of South Manchester. 7.2 The CCG continues to monitor and query the over 36 week waiters with the relevant providers. 7.3 There are no waiters over 52 weeks at month 7. Ambulance Contract 8.1 The Blackburn with Darwen CCG All Incidents activity of the ambulance service at Month 7 is above plan by 3.3%. 8.2 It is of note that although the activity in terms of response times for Blackburn with Darwen is performing strongly, it is the performance of NWAS overall that impacts on the CCG quality premium payment. For the quality premium performance NWAS as a provider is achieving 72.1% YTD against the target of 75% for Red 1 (%<8 mins). 8.3 The table below shows performance to date for Blackburn with Darwen. Blackburn with Darwen CCG – October 2014 Month ‐ Activity Year to Date ‐ Activity Activity % Status Activity % Status R1 (% <8 mins) 75% 46 78.3% G 390 80.5% G R2 (% <8 mins) 75% 798 80.8% G 5466 80.2% G All Reds (%<19 mins) 95% 844 94.5% R 5856 96.7% G Green 1201 ‐ ‐ 8904 ‐ ‐ AS3 7 ‐ ‐ 63 ‐ ‐ All Incidents 2052 ‐ ‐ 14823 ‐ ‐ Data Source: NWAS PES & HAS Reports Performance Line Target Plan 404 5,025 5,429 8,664 254 14,347 Comparison to Plan 14/15 Var 390 ‐14 5466 441 5856 427 8904 240 63 ‐191 14823 476 % Var ‐3.5% 8.8% 7.9% 2.8% ‐75.2% 3.3% CCG 14‐15 YTD Trend 9. Community Services – Lancashire Care NHS Foundation Trust 9.1 6 | P a g e Due to an agreed reporting pause for Quarter 3 in the contract year 2014-15, to support the assurance of the top 50 indicators provided by LCFT, there will be no data received and reported on until month 10. The quarter 3 data will be supplied in January 2015 in line with agreed timescales and will be broken down monthly. Monthly updates on progress will be shared by LCFT with Chorley and South Ribble CCG as the lead commissioner. 10. Other Community Services 10.1 The General Practitioners with Special Interests (GPwSI) work on a block contract basis. The activity performance against plan is in appendix 6 and shows activity variances against plan by provider. Commissioners continue to work closely with the GPwSI providers to monitor performance. 10.2 The Anticoagulation service is over plan for Community and Domiciliary by 18.4% and 33.3% respectively. 10.3 The Cardiology service is under plan for first appointments by 11.2% but over plan for follow ups by 64.3%. 10.4 The Diabetes service is under plan for first appointments by 57.1% but over plan for follow ups by 106.4%. 10.5 The Dermatology service is over plan in first and follow up appointments by 25.8% and 14.1% respectively. 10.6 The Ophthalmology service is over plan for first and follow up appointments by 38.9% and 7.4% respectively. 10.7 The Scheduled Care Team have undertaken a full review of the current GPwSI services across Blackburn with Darwen, in order to assure that they are delivering the desired outcomes and to inform on the future commissioning of these services. The review demonstrated that the GPwSI’s are providing services in line with quality and activity plans, noting some under and over performance. The services themselves are well received by patients, and patient engagement undertaken by the MLCSU has identified that patients value the services and the delivery of them, which aligns to the ‘Care Closer to Home’ strategy. 11. General Practice Out of Hours Service 11.1 The Out of Hours service is on a block contract with activity profiles based on a 2 year average of activity. The table below shows activity for Blackburn with Darwen. GP Out of Hours Service (ELMS) – October 2014 Year to date ‐ Activity 2014/15 2013/14 Variance Full Year Forecast ‐ Activity Status 2014/15 2013/14 Status PCC Attendances (Primary 6,752 Care Centre) 6,372 380 6.0% R 12,268 11,580 688 5.9% R Dr Advice 2,451 1,731 720 41.6% R 4,453 3,205 1,248 38.9% R Home Visits 1,608 1,464 144 9.8% R 2,922 2,597 325 12.5% R Total 10,811 9,567 1,244 13.0% R 19,642 17,382 2,260 13.0% R Data Source: Monitoring report provided by East Lancashire Medical Services (ELMS) 7 | P a g e Variance 11.2 The total activity is performing above plan when compared to the same period last year with the main increases in the Dr Advice and Home visits services. The detailed monthly performance is contained in graphical form in appendix 7. 12. Recommendation 12.1 The Governing Body is requested to note the contents of the report and the supporting appendices. Mr Roger Parr Chief Finance Officer 5 January 2015 8 | P a g e Appendix 1 BwD CCG GP Referrals to ELHT by Specialty – October 2014 (Year to Date) Specialty Number of Referrals Referrals per Working Day GP Referrals 2014‐15 GP Referrals 2013‐14 Variance Quantity Variance % 2014‐15 (149 days) 2013‐14 (150 days) Variance % General Surgery group 4 2841 2628 213 8.1% 19.1 17.5 8.8% E.N.T. 1637 1460 177 12.1% 11.0 9.7 12.9% T & O 1416 1278 138 10.8% 9.5 8.5 11.5% Other Specialty group 5 764 692 72 10.4% 5.1 4.6 11.1% Gynaecology 1804 1735 69 4.0% 12.1 11.6 4.7% Cardiology 839 776 63 8.1% 5.6 5.2 8.8% Rheumatology 408 366 42 11.5% 2.7 2.4 12.2% Dermatology 1172 1131 41 3.6% 7.9 7.5 4.3% Urology 852 819 33 4.0% 5.7 5.5 4.7% Obstetrics 1106 1094 12 1.1% 7.4 7.3 1.8% Paediatrics 571 560 11 2.0% 3.8 3.7 2.6% Pain Management group 123 6 General Medicine group 7 1483 147 ‐24 ‐16.3% 0.8 1.0 ‐15.8% 1496 ‐13 ‐0.9% 10.0 10.0 ‐0.2% Ophthalmology 1721 2206 ‐485 ‐22.0% 11.6 14.7 ‐21.5% Grand Total 16737 16388 349 2.1% 112.3 109.3 2.8% Data Source Ref: Referrals to Consultant‐Led clinics in ELHT Referrals dataset Definitions: GP Other Excluded Referrals into Consultant‐led clinic from a GP Referrals into Consultant‐led clinic from non‐GP medical professional (e.g. Consultant, Nurse Specialist) Referrals into Consultant‐led clinic from other sources (e.g. Self‐Referral, A&E department, Midwifery) Specialty Groupings General Surgery Group General Medicine Group General Surgery, Breast Assessment, Vascular Surgery General Medicine, Gastroenterology, Diabetic and Thoracic Medicine 9 | P a g e Appendix 2 There has been an increase in the Elective care over trade at month 7. ELHT have adjusted the activity profile for some specialties without prior agreement from the CCG. As a result, the contract monitoring performance summary for Elective will not be available until the month 8 report. 10 | P a g e Appen ndix 3 n Elective Activ vity (NEL + NEL LST) – BwD CCG G Patients at ELHT - Trend of Plan versus Ac ctivity 2010-11 to 2014-14 Non The cumulative Activity Volumes (6 mo onths) to Octoberr 2014‐15 are sligh htly above the acttivity levels seen in 2010‐11 (+0.6% %), 2011‐12 (+1.1% %) and last year 2013‐ 14 (++0.9%). However, year to date volumes are below (‐3.5%) the relativvely high levels experienced during the same period in 2012‐13. See below: 20 010‐11 : 10,477 sp pells 20 011‐12 : 10,431 sp pells 2012‐13 : 10,926 sp pells 20 013‐14 : 10,450 sp pells 20 014‐15 : 10,543 sp pells 11 | P a g e Appendix 4 Source : ELHT Performance Report Inpatient and Daycase Waiting List East Lancashire Hospitals Specialty General Surgery Urology Breast Care Orthopaedics ENT Ophthalmology Oral Surgery / Maxillo Facial Pain Management General Medicine Rehabilitation Cardiology Thoracic Medicine Nephrology Rheumatology Gynaecology Haematology Total Page 12 of 15 Current Month ‐ October 2014 0‐<6 Weeks 6‐<13 Weeks 13‐<20 Weeks 20 + Weeks 706 253 49 517 209 456 278 147 540 21 166 23 0 51 302 0 3718 194 71 17 195 83 252 103 103 2 14 14 0 0 17 43 0 1108 47 5 4 51 51 61 54 40 2 3 1 0 0 3 3 0 23 0 0 8 21 35 15 1 1 5 0 0 0 0 0 0 325 109 Grand Total Previous Month ‐ September 2014 0‐<6 Weeks 6‐<13 Weeks 13‐<20 Weeks 20 + Weeks 970 329 70 771 364 804 450 291 545 43 181 23 0 71 348 0 5260 659 230 43 460 218 453 307 184 487 8 143 24 1 31 270 0 3518 200 77 25 183 125 173 126 101 3 13 37 0 1 15 50 0 1129 56 5 2 58 68 47 46 31 1 6 1 0 0 3 4 0 13 2 0 17 25 27 27 1 1 4 0 0 0 0 2 0 328 119 Grand Total Variance 928 314 70 718 436 700 506 317 492 31 181 24 2 49 326 0 5094 %age +/‐ 42 4.5% 15 4.8% 0 0.0% 53 7.4% ‐72 ‐16.5% 104 14.9% ‐56 ‐11.1% ‐26 ‐8.2% 53 10.8% 12 38.7% 0 0.0% ‐1 ‐4.2% ‐2 ‐100.0% 22 44.9% 22 6.7% 0 N/A 166 3.3% Appendix 5 LCFT: Service Line Activity against Plan – October 2014 Due to an agreed reporting pause for Quarter 3 in the contract year 2014-15, in order to support the assurance of the top 50 indicators provided by LCFT, there will be no data received and reported on until month 10. The quarter 3 data will be supplied in January 2015 in line with agreed timescales and will be broken down monthly. Monthly updates on progress will be shared by LCFT with Chorley and South Ribble CCG as lead commissioner. Page 13 of 15 Appendix 6 General Practitioners with Special Interest (GPwSI) – October 2014 GPwSI Service Anti‐coagulation Cardiology Dermatology Diabetes Ophthalmology Activity Type Community Domiciliary First Follow‐Up First Follow‐Up First Follow‐Up First Follow‐Up Year to date ‐ Activity Plan Actual Variance 3,337 3,952 615 18.4% 758 1,011 253 33.3% 224 199 ‐25 ‐11.2% 56 92 36 64.3% 868 1,092 224 25.8% 609 695 86 14.1% 140 60 ‐80 ‐57.1% 140 289 149 106.4% 233 324 91 38.9% 175 188 13 7.4% Data Source: Spreadsheet data returns from individual GPwSI services. Page 14 of 15 Year‐on‐Year Comparison 14/15 13/14 Variance 3,952 3,412 540 15.8% 1,011 789 222 28.2% 199 162 37 22.7% 92 100 ‐8 ‐8.3% 1,092 939 153 16.3% 695 588 107 18.2% 60 100 ‐40 ‐39.8% 289 292 ‐3 ‐1.1% 324 268 56 20.7% 188 181 7 4.0% Appendix 7 O of Hourrs (OOH) Se ervice – Oc ctober 2014 4 GP Out BwD ‐ PCC A Attendance ((OOH) 2000 Bw wD ‐ Dr Advicce (OOH) 500 400 1500 300 1000 200 500 100 0 0 Apr M May Jun Jul Aug Sep Oct Novv Dec Jan Feb M Mar 2013‐14 Page 1 15 of 15 2014‐15 2012‐13 Apr May Jun Jul Aug Sep O Oct Nov Dec Ja an Feb Mar 2013‐14 20144‐15 20 012‐13 GOVERNING BODY MEETING Date of Meeting Title of Report Governing Body Responsible Officer Summary/Purpose Report Governing Body Action 14th January 2015 Agenda 12 Item No. Quality, Performance and Effectiveness Report Month 7 Dr Malcom Ridgway, Clinical Director for Quality and Effectiveness Lead Clinician Dr Malcom Ridgway, Clinical Director for Quality and Effectiveness Lead Mr David Rintoul, Quality and Manager Performance Specialist of This report provides the Clinical Commissioning Group (CCG) Governing Body with an update on the Quality, Performance and Effectiveness information of the main commissioned services as at October 2014, Month 7. The Governing Body is requested to note the contents of the report. Please indicate the Committee(s)/Group(s) where the paper has been discussed/developed Quality, Performance and Effectiveness Committee (QPEC) Please note the following section must be completed in full Patient and Public N/A Result Engagement Completed Equality Analysis N/A Completed Financial Implication(s) Nil Risk(s) Identified N/A CCG Strategic Objectives supported by this paper 1. We will continuously improve the health and well-being of the population of Blackburn with Darwen. 2. We will build successful partnerships which promote collaborative working and integrated service delivery. 3. We will effectively engage patients and the public in decision making. 4. We will co-commission and deliver continuous improvement in Primary Care Services and tackle inequalities. 5. We will commission safe and effective services for the population of Blackburn with Darwen with integration at the heart of commissioning. CCG High Impact Changes supported by this paper 1. Delivering high quality Primary Care at scale and improving access. 2. Self-Care and Early Intervention. 3. Enhanced and Integrated Primary Care and Better Care Fund. 4. Access to Re-ablement and Intermediate Care. 5. Improved hospital discharge and reduced length of stay. 6. Community based ambulatory care for specific conditions. 7. Access to high quality Urgent and Emergency Care. 8. Scheduled Care. 9. Quality. 1 | P a g e Y Y N/A Y Y N/A Y Y N/A Y Y Y Y Y CLINICAL COMMISSIONING GROUP (CCG) GOVERNING BODY MEETING 14th JANUARY 2015 QUALITY, PERFORMANCE AND EFFECTIVENESS REPORT MONTH 7 1.0 Introduction The following report contains information on CCG performance as well as provider quality performance against contractual obligations throughout the month of October 2014. The report focuses on exceptions and the progress of associated recovery plans and is collated from a range of sources; including but not limited to: provider board reports; Midlands and Lancashire Commissioning Support Unit (MLCSU) Business Intelligence; provider quality submissions; Clinical Commissioning Group (CCG) staff exception reports; as well as information from external bodies such as Health & Social Care Information Centre (HSCIC), NHS England; and Advancing Quality (AQ). Where appropriate, additional information focusing on other CCG patients is included; this is intended to provide a broader perspective for services where Blackburn with Darwen (BwD) CCG is the lead Commissioner. 2.0 Lancashire Care Foundation Trust – Mental Health Services 2.1 Improving Access to Psychological Therapies The notional 1.25% target for IAPT Prevalence was met in October 2014 for all CCGs except Fylde & Wyre (1.05%), with Trust performance at 1.46%. Prevalence for BwD CCG was 1.35% in October 2014, meeting the notional target; however, YTD performance remains below trajectory by 0.45%. The rebranding of the service, in an effort to reduce the stigma associated with accessing mental health services, is now underway and the new logo (below) will be used for all printed materials, such as new self-referral leaflets and promotional posters. The Trust continues to promote the self-referral pathway across all services in an effort to improve access for groups that might not traditionally engage with mental health services; for example, veterans, perinatal women, older adults, young men and Asian women. Recovery rates remain below the 50% target for all CCGs, at 36.1% in October 2014. The Trust has focussed resources on Prevalence and waiting times, which has impacted on Recovery rates. Sustaining a good Recovery rate is challenging due to areas of high deprivation within the region (e.g. parts of East Lancashire, Morecambe and Blackpool) meaning that more service users begin therapy with high symptom scores, and although patients may gain benefit from psychological interventions, the change in symptom scores may not be sufficient to take them below the level of “caseness” which is required for Recovery. Intensive Support Team work shows that if Clusters 1-3 can be the model client group (i.e. people with mid-range rather than severe conditions.), better recovery outcomes are predicted. IAPT services often fail to attract sufficient numbers of clients in the lowest clusters, which impacts on recovery rates. This is informing the Trust’s promotional work with the Trust seeking to appeal to people within lower clusters (e.g, the service’s rebranding to “Minds Matter”). 2 | P a g e 2.2 Memory Assessment Service The target for 70% of patients to be seen by the MAS within 4 weeks has not been met for any CCG area during October 2014. For BwD CCG, 32.26% of patients were seen within 4 weeks in October 2014, which is a decrease from a September 2014 performance of 57.50%. The average wait for BwD patients is currently 9.4 weeks, which is below the average wait across the whole service of 10.7 weeks. The Trust continues to work on reducing the backlog of patients waiting in an effort to reduce waiting times. For new patients, 69% are now seen within 4 weeks and LCFT are therefore confident that once the backlog is cleared, the Trust will be able to meet the 4 week requirement. LCFT have planned intensified work to clear the backlog in December 2014, and it is hoped that waiting time targets will begin to be met from January 2015. There also remains a significant number of referrals that do not have complete referral information (e.g. bloods). For example, for referrals received in October 2014, 25% still had missing information as of the 11th November 2014. This negatively impacts on waiting times in all areas that are affected by this issue. The Trust have made efforts to communicate with GPs where information at referral is outstanding and have discharged referrals back to GPs where information has been chased twice and still not completed. 2.3 Care Programme Approach 7 day follow-up Care Programme Approach (CPA) 7 day follow-up data has not been submitted for Month 7. Errors were highlighted by the MLCSU Quality and Performance team following the Month 6 data submission and, as a result, the Trust is currently in the process of validating CPA data. An update will follow in the Month 8 report. 3.0 Lancashire Care Foundation Trust – Community Services No issues have been reported with regards to the provider’s Month 7 Quality submission, however discussions are ongoing around the reporting criteria for Medicines Management following the Month 6/Q2 Quality submission. A meeting is also due to take place in December 2014 to discuss additional information required to reconcile the service’s 7 day working CQUIN scheme. 4.0 East Lancashire Hospitals Trust 4.1 18 Week Referral to Treatment Times Overall, the Trust is meeting the 18 weeks Referral to Treatment (RTT) standard; however, there were 4 specialties failing to achieve the 90% 18 weeks target in October 2014: ENT (83.8%), Urology (88.3%), Ophthalmology (88.7%) and Oral Surgery (83.0%). The host commissioner, East Lancashire CCG (EL CCG), continues to closely monitor performance. 4.2 A&E 4 Hour The 95% 4 hour target for A&E was not met in October 2014, with performance at 94.41%. Underperformance has been attributed to bed capacity and patient flow pressures within the Trust as well as short term staff sickness and surges in attendance at the Emergency Department (ED). Current improvement measures include: the purchase of 15 care home beds; the opening of Ward D1 for 48 hours each Monday to assist patient flow; the development of a live data feed of performance to support escalation; and the introduction of earlier discharges in the day (i.e. each ward to identify at least 2 patients suitable for discharge the following day; with these patients expected to be discharged between 10.00 and 13.00). 4.3 Clostridium Difficile ELHT is over trajectory for C. Difficile with the YTD position at 17 cases, against an annual YTD trajectory of 13 cases, there were no cases reported in October 2014. Post Infection Reviews (PIRs) are being undertaken for all cases, and are discussed across the health economy to highlight potential themes and trends. 4.4 Ambulance Handover – Hospital Arrival Screen Data Entry Compliance In October 2014 there were 338 breaches over 30 minutes and 10 breaches over 60 minutes, which is a decrease from the previous month. ELHT continues to meet weekly with North West Ambulance Trust (NWAS) management to raise and review performance on both sides and agree action. 3 | P a g e 4.5 Stroke 4 hour Despite consistent improvement earlier in the year against the 90% Local Quality Requirement target for Stroke Unit Admission within 4 hours, performance has deteriorated in correlation with wider A&E performance. 2013/14 year end performance was 50.46% and this had improved to 67.42% in August 2014; however, performance in October 2014 fell to 47.92%. The ring fencing of stroke beds on the Acute Stroke Unit (ASU) continues; however, bed pressures endure when medical bed capacity within the Trust is under pressure. Internal stroke improvement meetings continue to be held to review learning and breach analysis and a new Specialist Stroke Nurse has been recruited (start date to be confirmed) to support pulling patients through to the ASU. The Advancing Quality Appropriate Care Score, 60% target continues to be met, with performance in August 2014 at 65.00%, which is the latest validated position. 5.0 Calderstones Partnership Foundation Trust The CQC report following the inspection of CPFT in July 2014 has now been published and the Trust is due to develop an improvement plan. As the inspection was part of the new CQC Mental Health pilot, ratings have not been released. A further unannounced inspection is planned for 2015, for which, a formal rating will be published. A more detailed update will be available for the Month 8 report. 6.0 North West Ambulance Service The Red 1 and Red 2 emergency call response targets were met in October 2014 for BwD patients, at 78.51% and 80.80%. However, it should be noted that the CCG’s Quality Premium is linked to performance across the entire NWAS operational footprint for Red 1 calls on a YTD position, which is currently failing at 72.04%. The target for 95% of both Red 1 and Red 2 calls to be responded to within 19 minutes was also not met at both CCG and Trust level in October 2014, at 94.50% and 93.60%. Red call activity was 8% above plan for October 2014 (7.1% cumulative). NWAS has implemented a number of improvement measures including: additional funding to support performance and the utilisation of over time; weekly recovery meetings chaired by the Chief Operating Officer; an accelerated recruitment programme; and an Urgent Care Service demand review is to be undertaken against vehicle and staff availability, to increase capacity. 7.0 NHS Constitution A full breakdown of October 2014 NHS Constitution performance has been provided on the following pages 6 to 8, including exception information. 4 | P a g e 5 | P 5 age Period Target Oct 2014 Position Year to Date Position CCG Oct 2014-2015 0 0 0.00% CCG Q2 2014-2015 95.00% QTR 96.51% CCG Oct 2014-2015 0 0 1 CCG Jan 2013-2014 0 0 ELHT Oct 2014-2015 0 0 0 77: Number of G&A elective ordinary admission FFCEs in the period (77) CCG YTD 2014-2015 2,481 2,556 2,556 71: Number of G&A elective FFCEs in the period - Day Cases (71) CCG YTD 2014-2015 10,574 9,958 9,958 CCG YTD 2014-2015 11,947 11,784 11,784 CCG YTD 2014-2015 26,345 26,548 26,548 1926: A&E Attendances: Type 1 (1926) ELHT Nov 2014-2015 8,704 73,253 1927: A&E Attendances: All Types (1927) ELHT Nov 2014-2015 15,164 132,243 Metric Level NHS Constitution support m easures Mixed Sex Accom m odation Breaches 1067: Mixed sex accommodation breaches - All Providers (1067) Mental health 138: Proportion of patients on (CPA) discharged from inpatient care w ho are follow ed up w ithin 7 days (138) Referral To Treatm ent w aiting tim es for non-urgent consultant-led treatm ent 1839: Referral to Treatment - No of Incomplete Pathw ays Waiting >52 w eeks (1839) 1851: Referral to Treatment - Non-Admitted Pathw ays - No of Specialties Breached >52 Weeks (1851) A&E w aits 1928: 12 Hour Trolley w aits in A&E (1928) Activity Measures Elective Non Elective 72: Number of G&A non-elective FFCEs in the period - Total (72) Outpatients 73: All first outpatient attendances (consultant-led) in general and acute specialties (73) A&E 6 | P a g e 7.1 A&E waits Having met the 95% 4 hour A&E waiting time target at Trust level for the first four months of 2014/15, ELHT have failed the target in each of the following three months. October 2014 A&E 4 hour performance was 94.41% (please see section 4.2 on page 4). 7.2 Cancer waits - 31 days For the standard, 94% of patients to receive ‘subsequent treatment for cancer within 31 days (Surgery), although the BwD CCG YTD position is achieving the target at 97.52%, the target was not met for BwD patients in October 2014, at 93.55%. This related to two patients. 7.3 Cancer waits - 62 days The standard for 85% of patients to receive 1st definitive treatment for cancer within 62 days was not met for BwD patients in October 2014, at 80.49%, having achieved the target in September 2014 at 90.32%. The YTD position remains Red, at 82.30%. A recovery plan has been broadly agreed between ELHT, EL and BwD CCGs; however, certain elements require further agreement and negotiation. The maximum monthly number of breaches allowable for the remaining 5 months of 2014/15 is 4.4, with the average over 2014/15 to date being 5.6 breaches per month. The Strategic Clinical Network (SCN) position for the 62 day target is also failing at 84.2%. 7 of the 9 SCN Lancashire and Cumbria CCGs failed the 62 day target in Q2 (excluding East Lancashire and Greater Preston). This reflects overall declining performance. In Q1 2013/14, 4 CCGs failed and 5 achieved the 62 day target; yet over 6 subsequent quarters this has declined to 7 failing and 2 achieving. Over the same period, average performance across the 9 CCGs fell from 85% to 82.2% per quarter. Performance against the 62 day Cancer target continues to be actively scrutinised by the CCG’s Quality, Performance and Effectiveness Committee (QPEC). 7.4 Red 1 and Red 2 Category Ambulance The NWAS position remains red for the sixth consecutive month for both Red 1 (immediately life threatening) and Red 2 (life threatening but less time critical) emergency calls, at 71.20% and 72.04% against a target of 75%. The measure for 95% of Category A calls to be responded to within 19 minutes was also not met at Trust or CCG level, with performance at 93.60% and 94.50% (please see section 6.0 on page 5). 7.5 Activity Measures Activity measures have been provided as a high level overview only. Activity performance is covered in detail by the Contracting and Business Intelligence Report, which is available from Elaine Buckley, Contract Management Locality Lead. 7 | P a g e 8.0 Quality Premium 8.1 National Measures Domain(s) Measure Threshold Percentage of quality premium 15% Current month position 4,141.0 years (2013 position) Year to date position Potential years of life lost Achieve an agreed percentage reduction Available (PYLL) from causes in the PYLL between the 2013 and 2014 summer 2015 amenable to healthcare: calendar years adults, children and Demonstrate account taken of local young people factors An update is due to follow in the Month 8 report. Improving access to Achieve IAPT access levels of at least 15% 1.35% 8.30% Enhancing quality of psychological therapies 15% by 31 March 2015 life for people with (IAPT) (Notional target of 1.25% per month) long term conditions An update on progress for this indicator can be found on pages 21 to 22. Avoidable emergency A reduction or zero % change in 25% DSR 1744.2 Available Enhancing quality of admissions emergency admissions for identified summer 2015 life for people with conditions. long term conditions. The Indirectly Standardised Rate of Helping people to admission at less than 1,000 per 100,000 recover from population episodes of ill health or following injury. The table below shows progress on this indicator over time for Blackburn with Darwen. No Lancashire CCG is currently meeting the Directly Standardised Rate (DSR) target of less than 1,000 per 100,000 population. Looking at historic data only Blackpool met this target in 2010-11 and 2011-12 Preventing people from dying prematurely Period April 2013 – March 2014 2012-13 2011-12 2010-11 Ensuring that people have a positive experience of care 8 | P a g e Friends and Family Test and patient experience Female 1719.6 1876.1 1676.4 1432.8 Male 1769.0 1837.2 1595.8 1504.5 Agree a plan with local providers with specified actions and milestones Obtain appropriate assurance and evidence of action taken Support local providers to co-ordinate the Total 1744.2 1856.9 1636.7 1468.1 15% LCFT LCFT implementation implementation from January from January 2015 2015 Domain(s) Measure Threshold Percentage of quality premium Current month position Year to date position rollout of FFT Improved average score for one of the patient experience improvement indicators Clarification is being sought as to which provider the CCG will be measured against. An update will be provided in a future edition of this report. Improved reporting of Achievement of agreed increase in 15% Available Available Treating and caring medication safety reporting of medication errors from September September for people in a safe incidents specified local providers for the period 2014 2015 environment and Q4, 2013/14 and Q4, 2014/14 protecting them from avoidable harm Clarification is being sought as to which provider the CCG will be measured against. An update will be provided in a future edition of this report. 8.2 Local Measure Domain(s) Measure Threshold Percentage of quality premium 15% Current month position Gap of 135 Year to date position 58.6% Potential adjustment to funding -25% Current month position 96.11% Year to date position 95.54% -25% 94.41% 95.69% -25% 98.03% 95.61% Dementia Diagnosis Rate 67.04% diagnosis rate Enhancing quality of life for people with long term conditions Progress towards achieving this indicator is monitored through the Memory Assesment Service Performance Inprovement sub group. Further information can be found on pages 24 and 25. 8.3 NHS Constitution Measure NHS Constitution rights and pledges Referral to treatment times (18 weeks) A&E waits Cancer waits – 14 days 9 | P a g e Threshold Achieved for at least 92% of patients on incomplete non-emergency pathways over the course of the 2014/15 year Achieved for at least 95% of patients over the course of the 2014/15 year Measure based on a mapped proportion of ELHT patients Achieved for at least 93% of patients seen within 2 weeks from urgent GP referral to first Category A Red 1 ambulance calls 8.4 outpatient appointment over the course of the 2014/15 year Achieved for at least 75% of patients over the course of the 2014/15 year Measure based on NWAS performance across its operational footprint -25% 71.20% 72.04% Quality and Financial Gateways The CCG is required to demonstrate effective use of public resources while undertaking its business. Failure to do so will result in no Quality Premium payment being made. NHS England also reserve the right to not make any Quality Premium payment where they assess that the CCG is not considered to be making an appropriate and proportionate response to a local provider subject to enforcement action from the Care Quality Commission (CQC), Monitor or the NHS Trust Development Authority (TDA). Dr Malcolm Ridgway Clinical Director for Quality and Effectiveness 5th January 2015 10 | P a g e Date of Meeting Title of Report Governing Body Responsible Officer GOVERNING BODY MEETING Agenda 14th January 2015 15 Item No. Approval of further development of a scheme to provide intensive support to people living at home Lead Clinician Summary/Purpose of Report Dr Malcolm Ridgway, Clinical Director of Quality and Effectiveness Lead Mrs Lisa Kiernan, Head of Manager Primary Care and Integrated Community Services To inform Governing Body about the Pennine Lancashire development programme. Governing Body Action To seek approval for funding to extend the scheme that provides intensive support to people living at home. Approval of the Business Case Mrs Alison Shaw, Interim Programme Director Please indicate the Committee(s)/Group(s) where the paper has been discussed/developed Pennine Lancashire Chief Executive Officers BwD CCG Commissioning Business Group Please note the following section must be completed in full Patient and Public Yes Programme is part of communication underpinning winter Engagement and system resilience campaigns Completed Equality Analysis Yes PEAR completed Completed Financial Implication(s) In attached business case Risk(s) Identified In attached business case CCG Strategic Objectives supported by this paper 1. 2. 3. 4. 5. We will continuously improve the health and well-being of the population of Blackburn with Darwen. We will build successful partnerships which promote collaborative working and integrated service delivery. We will effectively engage patients and the public in decision making. We will co-commission and deliver continuous improvement in Primary Care Services and tackle inequalities. We will commission safe and effective services for the population of Blackburn with Darwen with integration at the heart of commissioning. X X X X CCG High Impact Changes supported by this paper 1. 2. 3. 4. 5. 6. 7. 8. 9. Delivering high quality Primary Care at scale and improving access. Self-Care and Early Intervention. Enhanced and Integrated Primary Care and Better Care Fund. Access to Re-ablement and Intermediate Care. Improved hospital discharge and reduced length of stay. Community based ambulatory care for specific conditions. Access to high quality Urgent and Emergency Care. Scheduled Care. Quality. X X X X X Page 1 of 21 GOVERNING BODY MEETING 14TH JANUARY 2015 PENNINE LANCASHIRE PROGRAMME 1. Introduction This paper provides a briefing on the 18 month pilot to test the impact of 3 of the schemes associated with delivering System Resilience and the Better Care Fund in 2014/15 and 2015/16 across Pennine Lancashire. 2. Background 2.1 Emergency admissions are rising across Pennine Lancashire, particularly in over 65’s. Older people stay in hospital longer than average and costs of admissions increase with age. More over 65’s are conveyed by ambulance, and of those conveyed 73% are admitted to hospital. 2.2 Both Blackburn with Darwen and East Lancashire CCGs have submitted Better Care Fund Plans which target approximately 2% reduction in emergency admissions from trend. The plans focus on support of the frail elderly in the first instance. 2.3 In July 2014, Chief Executives from Blackburn with Darwen Council, Lancashire County Council, Blackburn with Darwen and East Lancashire CCGs, Lancashire Care Foundation Trust and East Lancashire Hospitals Trust agreed to a set of principles to facilitate the development of a number of test changes to support system resilience and implementation of the Better Care Fund Plan objectives. The key strategic intentions for the development of the schemes across Pennine Lancashire can be summarised as follows: • • Initial focus for service redesign will be on complex frail elderly people Simplification of the system is vital leading to a minimal number of options with simple, single access points • Step up as well as step down as a feature of all Out of Hospital services • Discharge to assess long term care needs, allowing time outside of the acute setting to develop appropriate care plan for patients, relatives and carers Management of flow and capacity of the system needs to be co-ordinated and managed as a whole system • 3. Project Aims • • • • • • • Fewer people will be admitted to hospital as an emergency Quicker discharges and people will spend less time in hospital Fewer people will be admitted to permanent residential care Our system will be more easily navigated Fewer conveyances to Emergency Department System resilience will be maintained Improved patient and carer experience Page 2 of 21 3.1 The programme relates to services for complex frail adults and will initially focus on a test for change in 3 specific areas: • • • Care Navigation Hub and Directory of Services Intensive Home Support Discharge to Assess / intermediate care 4. Progress to date 4.1 Update on scheme development A specific work stream on communications has commenced that will focus initially on professionals use of the Directory of Services/ Hub and widen to ensure a greater understanding of out of hospitals services as they develop. 4.2 Navigation Hub and Directory of Services (DOS) The Care Navigation hub will provide a key interface with current services, Intensive Home Support and Discharge to Assess / intermediate care services. Alongside the hub a comprehensive DOS will provide advice, signposting and brokerage for health and care professionals to enable them to access the appropriate services for frail elderly patients. Progress includes: • • • • • • • A group of primary and secondary care clinicians together with colleagues from NWAS have tested the system using scenarios that reflect the range of need and clinical issues present in the frail elderly population. Testing has enabled enhancements to be made to the Directory and facilitated discussions with clinical staff in all providers The Directory of Services (DoS) has operational capability from 15th December onwards Focus is on step up from GP and Nursing Home sector with phasing in of A&E and MAU referral. The Pathway to services is being developed beginning with DoS to existing services and Intensive Home Support from February Specific communications for professional in relation to DoS are being developed The Phase 1 business case received approval by CBG on 10th December 2014. 4.3 Intensive Home Support The Intensive Home Support Service will be a community based, medically supported multidisciplinary team that focuses on the highest need patients at risk of a hospital admission or requiring intensive support following hospital discharge. It will provide rapid access to sub-acute and crisis care based on the needs of patients, and their carers supporting them to remain in their own home. The health and social care economy will work in partnership and in collaborative teams to deliver services. Page 3 of 21 Referrals will be able to be made direct by hospital and community through the Integrated Locality/Neighbourhood Teams or the Navigation Hub. The service is the very intensive element of integrated community provision in Blackburn with Darwen. Individuals will be supported for a maximum of 5 days and stepped into the most appropriate community service to ensure maximum flow and utilisation is achieved. Progress includes: • • • • • • Staff recruited to posts that will enable commencement of pilot on 2nd February 2015 Pathway developed that enables a maximum length of stay on Intensive Home Support of 5 days to ensure throughput and maximum utilisation On-going development of medical support to the pathway Work with local nursing homes in Blackburn with Darwen to ensure they are integrated into the scheme Review of virtual ward in East Lancashire to ensure additionality delivers the outcome of reduced conveyance to hospital. The business case with financial and activity modelling is attached for approval by Governing Body- Appendix 1 4.4 A ‘Discharge to Assess’ / intermediate care model is being developed and piloted. The pilot is initially testing a single model of step down care in Blackburn with Darwen that removes the current separation of health and social care beds. Progress includes: • • • • Stocktake of existing beds and usage Development of pathway to ensure that additional therapy capacity increases throughput and outcomes that ensure patients return to their own residence/ do not default to nursing home placement Development of test of change for an integrated discharge team- this includes rationalisation of team functions in and outside t h e h o s p i t a l b a s e a n d a n assessment pathway that enables a reduction in delayed discharges. Business case is to be developed once the delivery model is fully understood. 5. Risks and Deliverable Benefits The schemes will aim to deliver the following benefits which are consistent with our Better Care Fund submissions and our plans for system resilience: • • • • • Reducing unnecessary acute admissions and readmissions Reducing the length of stay in an acute bed Increasing patient choice and enhancing personalisation of care Reducing the number of patients discharged into residential care Increasing the number of patients who feel supported to manage their condition in their place of residence. Page 4 of 21 The risks are outlined in the table below Risk Extreme winter pressures impact on ability to achieve emergency admissions target Transformation change is not achieved within planned timescales Cultural shift in organisational thinking, delivery and decision making We do not have the right workforce with the right skills and capacity to deliver our plans including for 7 day services Financial risk – cost of community care is greater than acute episode We will not gain agreement from all partners for scale of pace required Mitigating actions Annual Resilience Plan monitored by the multi-agency Systems Resilience Group Existing governance structure includes providers and risks escalated accordingly through shared risk register, clear performance framework with KPIs in development Workforce development identified as a key enabler and plans will be progressed through Pennine Lancashire programme office As above Schemes will be piloted and phased delivery to enable evaluation of impact Plans have been jointly agreed by Pennine Lancashire Chief Executives 6. Impact of the Pilot 2014/15 – this period will focus on set up and mobilisation therefore we intend to maintain system resilience over the winter period 2015/16 - to delivery 2/3 of Better Care Fund Plan target for unplanned admissions from baseline (1000 across Pennine Lancashire. Approx. 600 for East Lancashire CCG and 400 for BwD CCG) 7. Governance Arrangements 7.1 Following the initial development and mobilisation of schemes the Executive Officers Group has reverted to its original development function working with the Pennine Lancashire Transformation Board to operationalise strategic clinical redesign. 7.2 A clinically led implementation group meets weekly to ensure introduction, review and monitoring of the Pennine Lancashire schemes. Representatives from provider organisations are supported by commissioners who will work to bring the scheme into a ‘business as usual’ position. 7.3 The implementation group reports to the Executive Officers Group and onwards to the Pennine Lancashire Chief Executives Group. The Chief Executives provide leadership and direction for the Pennine Lancashire programme and commissioning intentions and are currently considering the implications of the 5 Year Forward View for the health economy. 8. Recommendations Members are requested to approve the attached business case. Alison Shaw: Interim Programme Director: January 2015 Page 5 of 21 Non Recurrrent Funding Project Bus siness Cas se Appendixx A Nam me of proposed pro oject: In ntensive Home H Supp port Business C Case develloped by: Paula Fielld (LCFT) Date:Decem mber 2014 4 Business C Case supported by: Jamie Wa augh (LCFT T) PR ROJECT L LEADERSHIP: Prroject Sen nior Lead: Proje ect Manager: Claire Jacksson (Strattegic respo onsibility foor delivery)) Lisa Kiernan Prroject GP Lead: Proje ect Lead Accountan A nt: Dr D Malcolm Ridgway Gill Marr M Background to the proposal: Th he Pennin ne Lancasshire Healtth Econom my is a natural n foo otprint covvering the Boroughss of Blackburn w with Darwe en, Burnley y, Hyndburrn, Pendle e, the Ribb ble Valley aand Rosse endale. W hilst sttrong relationships exist e across health a and social care orga anisations in the area it has been b re ecognised that a morre formal arrangemen a nt would enable deve elopment oof a Pennin ne Lancasshire he ealth and care stra ategy and establish h a system m design blue prinnt that is resilient and su ustainable.. Th he system development is led by b the Pen nnine Lancashire Chief Executivve Officers s Group witth clinical advicce from the e Clinical Transforma T ation Board d. At the initial meetinng in June 2014 the Chief Execu utive Office ers agreed there wou ld be: • Colle ective owne ership of a transforma ation progrramme and d single plaan • An im mmediate requiremen r nt to identiffy the ‘quic ck wins’ wh hich would form part of o the progrramme and d a plan to design an nd impleme ent them. Th he aim of tthe project is to develop ideas i n the short, medium and long tterm to ens sure that pe eople are d diagnosed,, treated an nd cared fo or in the most m effectiv ve way; at least cost to the sy ystem. Ac cross Pennine Lanca ashire it ha as been a agreed thatt any chan nges to sysstem chan nge must build b on n, and nott duplicate or introdu uce comple exity into the existing g system. All system m changes will be e responssive to our ongoin ng develo pment of integrate ed locality//neighbourrhood tea ams; integrated d discharge and the re emodel of the entire e intermediate care ssystem aligned to CCG C sttrategic and d operation nal plans and a agreed d Better Ca are Fund sc chemes. Im mproved qu uality of ca are and in n particularr patient experience e is the keyy driver fo or this servvice re edesign. 1 Page 6 6 of 21 The strategic objective of the Pennine Lancashire initiatives are detailed in the Cases for Change for both BwD and East Lancashire CCGs and the principles can be summarised as follows: • Simplification of the system is vital leading to a minimal number of options with simple, single access points. • Clear separation of Acute Hospital and Out of Hospital services • Step up as well as step down for all Out of Hospital services. • Discharge to assess long term care needs from acute care, allowing time to think for patients, relatives and carers. • Management of flow and capacity of the system needs to be co-ordinated and managed as a whole system. • Trust in the robustness of the Out of Hospital system has to be established. • Capacity has to be available and greater flexibility of the system is required, specific to the needs of the person • Response has to be quick when needed and must be 7 day. • Assessment needs to be trusted rather than repeated with exclusion criteria removed. • Robust medical oversight is required. • Full spectrum of need will be addressed from light touch through to intensive support. • Predominantly frailty related initially. BWD IHS Outline Business CaseDec14dec14 Blackburn with Darwen Intensive Home Support Service Executive Summary The purpose of this business case is to obtain agreement to the commissioning of a ‘step up’ admission avoidance service for the Blackburn with Darwen health economy to be provided by Lancashire Care Foundation Trust. The service will facilitate proactive prevention & early intervention, out of hospital care, to meet the physical, mental health & social care needs of frail elderly patients to empower and support them to live independently in their own homes. The Intensive Home Support service is a medically led, multi-disciplinary team with dedicated pharmaceutical & social work provision. It will work in collaboration with existing physical & mental health teams to facilitate a seamless patient pathway on a step-up basis The pilot phase will commence in February 2015 with a phased implementation which will deliver 14 virtual beds when fully operational in May 2015. The following is a high level summary of finance and activity and reflects 3 years data to evidence the increased savings potential from year 2. More detail is shown in financial and activity analysis and appendix C. Admissions Saved Year 1 783 Year 2 1,040 Year 3 1,040 Savings £532k £948k £917k 1) Project Aim(s) The service will facilitate proactive prevention & early intervention, out of hospital care, to meet the physical, mental health & social care needs of frail elderly patients to empower and support them to live independently in their own homes by: Collaborating with Integrated Neighbourhood Teams to identify patients who require an intensive service, on a step-up basis, to prevent a hospital admission Using a community based multi-disciplinary team, wrapping services around the needs of the patient Providing a holistic assessment of need and necessary support, equipment and interventions to promote stability in the patient’s condition Preventing an avoidable admission to hospital by providing support and therapeutic interventions during acute illness or sudden deterioration in condition Providing a rapid access, high quality ‘step-up’ service that meets the needs of those at risk of a hospital admission Preventing unwarranted admissions into short-term residential care beds BWD IHS Outline Business CaseDec14dec14 Actively develop close working relationships with partner organisations, e.g. health, social, VCFS & NWAS, housing providers to maximise patients to remain at home, where appropriate Reduces duplication of assessment 2) Deliverable Benefits The services main objectives include: reducing unnecessary acute admissions and readmissions increasing patient choice and enhancing personalisation of care increasing the number of patients who feel supported to manage their condition in their place of residence In order to meet the objectives the service will need to: Retain medical responsibility for the patients whilst in the service Be medically led by a fully accountable generalist doctor Be provided by a multi-disciplinary, community based team Integrate with existing physical and mental health provision & social care; including the direct commissioning of re-ablement and crisis offer Be accessible & responsive to meet the needs of referrers Validate a ‘Trusted Assessment’ to ensure appropriateness of case mix and undertake assessment when needed Provide full medicines management reconciliation to prevent negative polypharmacy & pill burden Ensure sharing of information regarding management plans and interventions Ensure regular caseload reviews take place in primary health care settings within the MDT of the Neighbourhood teams BWD IHS Outline Business CaseDec14dec14 3) Service Delivery The Intensive Home Support service is a medically supported, multi-disciplinary team with dedicated pharmaceutical & social work provision. It will work in collaboration with existing physical & mental health teams to facilitate a seamless patient pathway on a step-up basis as detailed below: BWD IHS Outline Business CaseDec14dec14 This service provides an admission avoidance scheme. As required by the CCG, the first phase of implementation will focus on preventing the admission of patients in nursing homes. This will commence in February 2015. Patients will be ‘stepped-up’ from nursing homes in Blackburn with Darwen onto the Intensive Home Service. A roll-out of step-up from the patient’s own home will follow. In collaboration with East Lancashire Hospitals NHS Trust, patients will be stepped-up from the ‘front door’ of the acute hospital, working in conjunction with teams in the Urgent Care Centre & Emergency Departments to support the identification of clinically appropriate patients to admit to the Intensive Home Support Service. It will enhance & identify any required redesign of current processes to facilitate effective & co-ordinated care across the health economy. Cognisant that the Integrated Locality Teams (ILTs) are essential to the effective delivery of this service, robust collaborative clinical pathways will be developed to ensure patients are stepped up into the IHS & stepped down to the ILT as clinically appropriate. To facilitate this, a Trusted Assessment will be carried out by ‘Trusted Assessors’ identified from existing acute & community teams to support the seamless coordination of the patient’s pathway. It is planned that the ILTs will be trained as Trusted Assessors in the initial stages of roll out. Acute Bed Intensive Home Support Integrated Locality Teams 4) Performance Monitoring Integral to the successful implementation & delivery of Intensive Home Support, is the supporting technology & infrastructure to support it. This operational infrastructure supports the following: • • • 24/7 nurse triage & helpline Live patient activity & case notes Scheduling of appointment BWD IHS Outline Business CaseDec14dec14 • Robust activity & performance management data Our system will capture both the inputs, outputs & outcomes for patients referred onto the service. Reporting is expected to capture the following, however, is not an exhaustive list. • • • • • • • • • Referring clinician Referral route Number of patients referred into IHS Number of patients accepted Diagnosis/presenting complaint Number of days remaining on service Discharge destination Number of patients ‘rejected’ and reason why Detail of alternative service patient navigated to It is expected that a number of performance reports will be generated to include the following information: • • • • number of admissions avoided & length of stay number of patients accepted on service and number of patients discharged each day response times patient satisfaction It should be noted that this is not an exhaustive list. It is expected that pre & post implementation, LCFT will work closely with commissioners to identify the detailed information required to support the evaluation of the pilot to inform the future planning and procurement requirements. 5) Rationale for IHS This additional service is required to deliver the culture, capacity & competency shift required to deliver significant change. Lancashire Care NHS Foundation Trust is unable to provide this within its existing services owing to the pressures in the health economy to achieve radical change in a short length of time. LCFT intends to sub-contract this service, whilst integrating with current services to demonstrate & share the benefits of working in a different way to achieve significant change. This gives LCFT the opportunity to learn from a provider who has achieved success with this model & shape its services accordingly. It should be noted, that the IHS will work in a seamless way with existing services to provide the shared learning & development required for a sustainable out of hospital service offer. The service will be truly integrated including medical responsibility, social worker, mental health services together with a multidisciplinary nursing & therapy team wrapped around the holistic needs of the patient. BWD IHS Outline Business CaseDec14dec14 6) Key Partners • • • • • • • • • Blackburn with Darwen General Practices Lancashire Care Foundation Trust Care Homes and Nursing Homes Blackburn with Darwen Borough Council Lancashire County Council NWAS Voluntary Community Faith Sector East Lancashire Medical Services East Lancashire Hospitals Trust 7) Scope In Scope: Blackburn with Darwen registered patients who are identified as appropriate for out of hospital care and whose care package is identified as requiring Intensive Home Support Out of Scope: Initially, non-Blackburn with Darwen registered patients Patients whose care package can/should be provided by existing community service 8) Timescales – Key dates Project Start Date: Mid October 2014 Checkpoint 1: Mid-November 2014 Checkpoint 3: Mid-May 2015 – Service review Please see appendix A for more detailed timeline BWD IHS Outline Business CaseDec14dec14 Project End Date: 31st December 2015 Checkpoint 2: End January 2015 Checkpoint 4: Mid October 2015 Non Re ecurrent Funding Projectt Business Cas se App pendix A 9) FINA ANCIAL AND A ACTIVITY APP PRAISAL PLEASE E NOTE THES SE COSTS ARE E EXCLUSIVE E OF ADDITION NAL COSTS RELATING R TO MEDICAL M PRO OVISION, BASED ON THE ASSUM MPTION THAT COMMISSION NERS HAVE ADVISED LCFT T TO WORK WITH CURRENT T SERVICE PR ROVIDERS. Financiial Implication ns Year 1 ((Feb 2015 to Ja an 2016) Disaggrregated to Feb--Mar 2014-15 Year 2 ((Feb 2016 to JJan 2017) Year 3 ((Feb 2017 to Ja an 2018) Gross (totall) cost to deliv ver the scheme e £962k inc £8 85k set up costts £200k inc £8 85k set up costts £1,036k £1,067k Gross s (total) saving gs to deliver the sc cheme £1,494 4k Net Savings (Total Savings s less total costs) £532k £1,984 4k £1,984 4k £948k £917k Notes The cossts above do no ot include any additional a costss of prescribed d drugs outside e what the patie ents will have already a been prrovided by theirr GP The savvings are based d on avoiding emergency e adm missions as sta ated in the activ vity table in app pendix B provid ded by the CCG G The unitt cost stated byy the CCG for an a emergency admission is £ £1,908 Year 1 ccosts, savings and activity are e lower than ye ears 2 and 3 du ue to the phase ed implementattion of the serv vice Not included in the abo ove savings arre the costs of a any associated d A&E attendan nces/re-attenda ances and follo ow up appointm ments Activity y Implications Year 1 ((Feb 2015 to Ja an 2016) Year 2 ((Feb 2016 to Ja an 2017) Year 3 ((Feb 2017 to Ja an 2018) Number of Virtual Beds s 14 14 14 Average e Length of Stay (da ays) 5 5 5 Admissions eek Saved Per We 20 20 20 Admissions P Year Saved Per 7 783 1,0 040 1,0 040 Please see appendix C for detailed roll-out r plan & a activity – which h demonstrates s the total numb ber of admissio ons is in line witth commissioner ptions. Robust monthly perforrmance monito oring will suppo ort the reconcilia ation of these assumptions a ag gainst activity planned. p assump 9 Non Recurrrent Funding Project Bus siness Cas se Appendixx A 10 0) Workforce To o deliver th he service as outlined d above th here will be e a requirem ment of addditional ca apacity to prrovide support to the existing health and social serv vices. This will be acchieved through the prroactive exxternal recrruitment off additionall staff. Th he service will require e a change e in some methods of o current practice p as well as the e way in which teamss across th he health and a social ccare econo omy work together too co-ordinate care pa athways. In n order to achieve a this there is a phased introductio i n to servicce delivery which allows th he balance of providin ng time forr changes tto be introd duced and embeddedd whilst als so beginnin ng to o deliver the e benefits to the patie ent. It is assume ed that exissting knowlledge, skillls and expe erience witthin the heealth and so ocial care ec conomy will enable fa ast and efffective servvice mobilis sation and delivery. 11 1) Estates s/Infrastruc cture Th here is a re ecognition that to ena able all rele evant prov viders across Blackbuurn with Da arwen to work w to ogether the ere is a more detailed d piece of w work requirred to unde erstand thee IT solutio ons needed d which will en nable partn nership wo orking acro ss organis sations. This is flaggeed as a risk k to the prroject. Th here are no o estates implications for the C CCG in prov viding an Intensive H Home Supp port service e 12 2) Quality Staff will: Monittor the effe ectiveness of clinical practice th hrough the quality asssurance sttrategies su uch as the e use of au udit and pe eer review Mainttain professsional registration Particcipate in co ontinuing professiona p al development oppo ortunities too ensure th hat up-to-d date evide ence-based d knowledg ge and com mpetence in i all aspec cts of roless is maintained Workk within the e latest NM MC Code off Professio onal Condu uct Reco ord accuratte consulta ation data in patients s records in n accordannce with th he latest NMC guida ance and other o pertin nent standa ards Keep p up to datte with pertinent hea alth-related d policy an nd work w ith the Loc cality team m to consiider the im mpact and strategies s ffor implementation Workk collaborattively with colleaguess within an nd external to the Loccality. Enco ourage and develop te eamwork w within the Locality. L Particcipate in multi-discipl m inary proto ocol and Patient Grou up Directioons development 10 13) Key Performance Indicators First line metrics and Key performance indicators have been agreed as follows: Provider Activity Frequency of reporting Performance Target Number of admissions avoided Monthly Total number of referrals Source of referral Total number of assessments Total number accepted on programme Total accepted on programme were admission would have been action of referrer Utilisation of IHS beds % of capacity utilised Monthly Length of stay on IHS Average length of stay on IHS programme Monthly Quality Target Discharge Monthly Number and % discharged to primary care Number and % admitted to secondary care Number and % deaths expected (palliative) a 14) Alternative options Elements of an Intensive Home Support service already exist and are successful e.g. East Virtual Ward pilot, however to provide the holistic model required, a significant step-change is required. BWD IHS Outline Business CaseDec14dec14 15) Impact Assessment Area Primary Care X Community Care X Secondary Care X Social Care X Voluntary Sector X Other (please state) X Details regarding impact and engagement/consultation which has taken place Engagement with practices has been through face to face meetings at the Senate and at each of the 4 locality group meetings. Primary care will be able to refer patients to IHS to prevent a hospital admission. Collaborative working with the Acute Visiting Scheme will free up primary care capacity to deliver core business Represented at the Executive Officers Group. LCFT will deliver the physical nursing & therapy elements of the service in collaboration with current mental health services. This will require additional workforce capacity to provide a quick responsive 7 day service that is capable of addressing the full spectrum of patient need. Represented at the Executive Officers Group. The main objectives of the IHS service include preventing a hospital admission/readmission via step up provision. Represented at the Executive Officers Group. Social Care will form an integral part of HIS, providing social care assessments and reablement as part of the multi-disciplinary team approach. Represented at the Executive Officers Group. The voluntary sector will provide support to those patients on IHS via self-care support etc. NWAS & ELMS – both organisations are represented at the Executive Officers Group. NWAS will be able to refer patients to IHS to prevent hospital admissions. Early discussions have commenced with ELMS & the CCG to facilitate AVS providing the medical cover for the IHS service. 16) Interfaces • Internal Integrated locality teams – the ILTs are a key component of overall service delivery. The IHS will work seamlessly with ILTs to provide a step-up/step-down service for patients as clinically appropriate IST & Care Home Liaison – pathway development to facilitate collaborative working between the IHS & our mental health services will provide a holistic model of care for patients. It delivers a positive outcome for both our patients and LCFT. Joint working will facilitate the development of additional competencies across our physical and mental health teams. Medicines management – will form part of the IHS MDT team to provide full medicines management reconciliation to prevent negative polypharmacy and pill burden. Current LCFT services – gives LCFT the opportunity to review & redesign existing services whilst developing its capacity, competency & capability to deliver the IHS. BWD IHS Outline Business CaseDec14dec14 External Acute Visiting Scheme – the CCG has advised that we work with the existing service in the pilot phase to provide our medical oversight. The impact on AVS capacity is currently unknown but will be measured throughout the lifetime of the service mobilisation and ramp up. Primary care – the IHS offers GPs an alternative, where clinically appropriate, to a hospital admission. GPs will feel supported in the knowledge that their patients are being kept safe, under separate medical leadership, whilst in the care of the Intensive Home Support service. 17) Interdependencies For this service to operate successfully, all partners identified above will need to commit to working together to maximise patients to remain at their place of residence. This is likely to mean sharing best practice, creating a trusted assessment that can be used across health and social care, access to shared IT systems and collaborating to design service and referral pathways across Blackburn with Darwen. The development and agreement of a robust governance structure to support a dedicated medical model is key to the success of the project. 18) Risks Insufficient lead-in time to mobilise service delivery to reduce pressures for winter Partners are unwilling to support IHS Medical model has still to be agreed Unable to recruit additional capacity needed leading to delay in service delivery IT issues unable to be addressed or too costly Not enough time to be able to understand the complex care and referral pathways resulting in inefficiencies Lack of clearly defined scope and specification Assumptions relating to demand & capacity modelling have not been able to be validated due to the lack of supporting evidence and data 19) Agreement to Proceed Name Project Senior Lead: Project Manager: Project GP Lead: Project Lead Accountant: Date business case reviewed BWD IHS Outline Business CaseDec14dec14 Signature Outcome Date Non Re ecurrent Funding Projectt Business Cas se App pendix A 14 ELEMENT SIX Activity, Bed Day and Cost Impacts of Step Up into Intensive Home Support (HIS) [Indicative] Activity LOS Cost Average LOS Average Cost Activity LOS Cost Average LOS Average Cost Activity LOS Cost Average LOS Average Cost Activity LOS Cost Average LOS Average Cost Activity LOS Cost Average LOS Average Cost TOTAL [4] 20+ days [3] 10‐19 days [2] 3‐9 days [1] 0‐2 days LOS £ £ £ £ £ £ £ £ £ £ 2013‐14 Emergency Admissions BwD CCG EL CCG PENNINE LANCS 1950 4923 6873 1436 3694 5130 1,765,777 £ 4,521,187 £ 6,286,964 0.74 0.75 0.75 906 £ 918 £ 915 1400 3483 4883 7554 18570 26124 3,371,709 £ 8,639,013 £ 12,010,722 5.40 5.33 5.35 2,408 £ 2,480 £ 2,460 557 1147 1704 7424 15289 22713 1,621,468 £ 3,266,479 £ 4,887,947 13.33 13.33 13.33 2,911 £ 2,848 £ 2,869 303 955 1258 10798 36152 46950 1,274,081 £ 3,599,926 £ 4,874,007 35.64 37.86 37.32 4,205 £ 3,770 £ 3,874 4210 10508 14718 27212 73705 100917 8,033,035 £ 20,026,605 £ 28,059,640 6.46 7.01 6.86 1,908 £ 1,906 £ 1,906 Source Secondary Uses Service Spell Data ‐ MLCSU Data Warehouse BWD IHS Outline Business CaseDec14dec14 STEP UP IMPACT 50% Activity, Bed Day and Cost Impact [Indicative] BwD CCG EL CCG PENNINE LANCS 975 2462 3437 718 1847 2565 £ 882,888 £ 2,261,053 £ 3,143,941 STEP DOWN LOS Impact 0% 0 15% £ 210 1133 505,756 £ 522 2783 1,294,736 £ 732 3916 1,800,492 Activity, Bed Day and Cost Impact [Indicative] BwD CCG EL CCG PENNINE LANCS 0 0 0 0 0 0 £ ‐ £ ‐ £ ‐ 0.74 0.75 0.75 140 280 10% 2 £ 5% £ 28 373 81,510 £ 57 760 162,327 £ 85 1133 243,837 25% 3 5% £ 15 535 63,073 £ 48 1817 180,939 £ 63 2352 244,012 40% 8 £ 1228 2759 1,533,228 £ 3089 7207 3,899,054 £ 4317 9966 5,432,283 £ £ ‐ £ ‐ 3.33 3.35 139 458.7 287 947.1 426 1405.8 ‐ £ ‐ £ ‐ 10.03 10.03 10.03 121 968 382 3056 503 4024 £ ‐ 488 976 3.40 £ 348 696 ‐ £ ‐ £ ‐ 27.64 29.86 29.32 400 1706.7 1017 4699.1 1417 6405.8 ‐ £ ‐ £ Bed Impact [100% / 365 days per annum] 7.56 19.75 27.30 Bed Impact [100% / 365 days per annum] 4.68 12.87 17.55 ‐ Blackburn with Darwen – Intensive Home Support Implementation Schedule Month 2015 Virtual Beds Admissions Saved Bed Nights Saved BWD IHS Outline Business CaseDec14dec14 Feb Mar Apr May Jun July Aug Sep Oct Nov Dec Jan 16 3 6 8 14 14 14 14 14 14 14 14 14 18 36 49 85 85 85 85 85 85 85 85 85 92 184 246 430 430 430 430 430 430 430 430 430 GOVERNING BODY MEETING Date of Meeting 14th January 2015 Agenda Item No. 16 Title of Report Healthier Lancashire Purpose Document Governing Body Responsible Officer Summary/Purpose of Report Lead Dr Chris Clayton, Clinical Chief Clinician Officer Lead Manager This document is structured in three sections; section one sets out the Healthier Lancashire journey from the first paper to the three Health and Wellbeing Boards, to the Lancashire Leadership Forum’s agreement to establish a programme of work to bring about change across the Lancashire health and social care system, right up to the present day with the desire to move forward to develop and deliver a strategic plan. Dr Chris Clayton, Clinical Chief Officer Section two aims to set out some of the evidence that supports the need for change and has been derived from the Sustainability Assessment Framework (SAF) that the Leadership Forum commissioned from Oliver Wyman. The third and final section is intended to describe the proposal for creating a system wide programme of work. The first phase of which would be a strong process to develop a strategic plan for Lancashire by the end of May 2015. The Healthier Lancashire Team has co-ordinated the compilation of this document to summarise the essence of discussions and decisions taken by the Healthier Lancashire Executive and Lancashire Leadership Forum since the beginning of September 2014. In establishing the Healthier Lancashire Programme, the Leadership Forum recognised the challenges associated with improving outcomes and that these cannot be met by one organisation alone. This document is all about ensuring that the Healthier Lancashire Programme is co-designed and engages people through strong relationships and commitment. It is hoped therefore, that it can be used to support discussions to ensure that all the organisations which are members of Healthier Lancashire feel engaged in and informed about the work to date and the planned activities for early 2015. The Leadership Forum in February will continue the journey with detailed discussions about the process for developing a Strategic Plan. Governing Body Action The Governing Body is requested to consider and submit views on the content of the purpose document to be fed back to the Lancashire Leadership Forum in February. Please indicate the Committee(s)/Group(s) where the paper has been discussed/developed Lancashire Leadership Forum Page 1 of 2 Please note the following section must be completed in full Patient and Public N/A (if yes, complete outcome) Engagement Completed Equality Analysis N/A (if yes, complete outcome) Completed Financial Implication(s) N/A Risk(s) Identified N/A CCG Strategic Objectives supported by this paper 1. 2. 3. 4. 5. We will continuously improve the health and well-being of the population of Blackburn with Darwen. We will build successful partnerships which promote collaborative working and integrated service delivery. We will effectively engage patients and the public in decision making. We will co-commission and deliver continuous improvement in Primary Care Services and tackle inequalities. We will commission safe and effective services for the population of Blackburn with Darwen with integration at the heart of commissioning. Y Y Y Y CCG High Impact Changes supported by this paper 1. 2. 3. 4. 5. 6. 7. 8. 9. Delivering high quality Primary Care at scale and improving access. Self-Care and Early Intervention. Enhanced and Integrated Primary Care and Better Care Fund. Access to Re-ablement and Intermediate Care. Improved hospital discharge and reduced length of stay. Community based ambulatory care for specific conditions. Access to high quality Urgent and Emergency Care. Scheduled Care. Quality. Page 2 of 2 N/A Y Y Y Y N/A Y Y Y Healthier Lancashire Programme Purpose Document A Lancashire System Response to the Five Year Forward View December 2014 Healthier Lancashire Programme “All Lancashire people are united around a common cause; one that stops people from being patients” The Healthier Lancashire mission… “To lead the way in an unprecedented collaboration between people and organisations to define a new and better future for health and care in Lancashire” 2 ‘ The programme has a clear vision… Purpose Document A Lancashire System Response to the Five Year Forward View Contents INTRODUCTION The origins of Healthier Lancashire The Purpose of this document Strategic context There are mounting demands on care budgets The NHS “Five Year Forward View” An emerging consensus within Lancashire Lancashire - demographics and geography The strategic challenge The moment of opportunity WHERE WE ARE STARTING FROM Lancashire has an ageing population Residents in Lancashire are less healthy than the national average Many Lancashire people have three or more long-term health conditions (LTCs) Lancashire residents are also more likely to die early There are significant health inequalities within Lancashire Health services struggle to meet current performance targets Patient experience is variable Staff satisfaction is deteriorating There are also big workforce challenges While demand for health and social care services is growing Social care has challenges too The third sector is not adequately financed to fill the gaps CREATING A SYSTEM WIDE PROGRAMME Why a Strategic Plan? What is a Strategic Plan? A Strategic Plan for All Lancashire Leadership Organising Timetable Mobilising the Strategic Plan Underpinning Communication and Engagement Strategy for the Strategic Plan CONCLUSION GLOSSARY OF KEY TERMS REFERENCES This document has been prepared on behalf of the Lancashire Leadership Forum in partnership with Oliver Wyman, a global leader in management consulting, and Freshwater UK, an integrated communications consultancy. The content has been complemented by the stakeholder activities designed and facilitated by True North Communications Limited. 3 Healthier Lancashire Programme Introduction The origins of Healthier Lancashire In Lancashire, there has been some history of close collaboration between health and care organisations and Councils, but there has been a collective frustration that it has not delivered the anticipated outcomes. Following the implementation of the Health and Social Care Act 20121 the Lancashire Leadership Forum was created with representation from the three top tier Local Authorities, Clinical Commissioning Groups, Provider NHS Trusts, Health Education England, HealthWatch, the third sector, Public Health England and NHS England. The Leadership Forum agreed to create a Lancashire level health and care strategy, called “Healthier Lancashire” following two workshops in autumn 2013. This was followed by a paper presented by the Area Team Medical Director, on behalf of the Leadership Forum, to the three Health and Wellbeing Boards. Subsequently, a Programme Director was appointed, supported by a Programme Team. NHS England has provided the initial non-recurrent funding which has covered the establishment of the Programme, and the development of this Purpose Document and the future development of the Strategic Plan. The purpose of this document The Purpose Document is intended to set out the journey to date and the proposed next phase of development. It is designed to confirm the scope, align plans and set out priorities for action. This work will be undertaken within a legally robust governance framework, follow best practice processes and will ensure a consistency of approach. In establishing the Programme, the Leadership Forum recognised the challenges associated with improving outcomes. These cannot be met by one organisation alone and strategic planning needs to be worked through at a Lancashire level to build a sustainable health and care system. However, it is understood that need varies across the county and this will not be a one-size-fits-all strategy. Healthier Lancashire will align with and add value to the strategies of the Health and Wellbeing Boards and the two and five year plans of our CCGs and Provider Trusts, including the Better Care Fund. While there must be clear and transparent standards of care across the whole of Lancashire, the response and delivery of these standards will be tailored to meet local need and will build on existing successes. This document has been produced to stimulate a wider discussion across the health and care system, reflecting the extensive engagement that has taken place over the past few months. The discussions are expected to lead to a reaffirmed commitment to the next stage of the work. The Strategic Plan will detail opportunities for collaboration within Lancashire and within local health and care systems. It mirrors the ambition and desire for change that has been apparent in discussions over the past few months, never more so than at the summit held at Turf Moor in November. 4 Purpose Document A Lancashire System Response to the Five Year Forward View This document is all about ensuring that the activities within the Programme are co-designed and engage people through strong relationships and commitment. By people, this means the leaders of Lancashire organisations, all the staff that work within health and care - in the statutory, third and private sectors - that contribute to health and wellbeing. The document is written for the Boards and Governing bodies of Lancashire’s health and care organisations, although it will also be discussed on a wider level. Strategic Context The health and care system, nationally and locally, continues to be exposed to number of significant challenges including; evolving needs and demographic trends, emerging technologies, and the political landscape. With these challenges comes great opportunity. The NHS has been variously described as one of “the most trusted organisations in British society”, our “proudest achievement” and “the envy of the world”. It is not just a great institution but a unique expression of a noble ideal - that healthcare should not be a privilege to be purchased but rather a moral right available to all. As we acknowledge and celebrate the achievements of the NHS we must also address the health and care challenges of the future to build a fully integrated, collaborative system. The problems that the NHS faces cannot be solved by the NHS alone. Nationally these issues have recently been addressed in the NHS Five Year Forward View2 which notes that while the values of the NHS are unchanging, the service itself must change if it is to meet the needs of the people in a rapidly evolving world. 5 Healthier Lancashire Programme The proposal made to the Health and Wellbeing Boards for a Healthier Lancashire Programme was largely borne out of a shared recognition of the need to transform the poor outcomes that are outlined in Section Two, titled ‘Where we are starting from’. The health and care system continues to grapple with the challenges of finite resources, growing demand, changing health needs and the public requirement for greater information and more involvement. There is a growing sense that “We can’t go on like this” but there are differing views as to what exactly “this” is. For some people it is principally about tackling poor health outcomes, for others it is a question of unsustainable service models and for others still it is a matter of changing health needs. In truth, all of these factors mean we cannot carry on as we are. If we do not address these challenges we will not be able to maintain the comprehensive, high quality NHS the people of Lancashire clearly want. There are mounting demands on care budgets… There is evidence that investing in spending on the right kinds of social care can reduce the strain on the wider health and care system – by avoiding unnecessary admissions and reducing the length of hospital stay where appropriate. However, preventative services and social care often become a low priority when resources are squeezed. Councils have been working closely with the health and care system to support the increasing numbers of people who leave hospital every week. They have also had to cut back on free adult social care and many local councils feel that the scope for further savings is now reduced. By 2020, it is predicted that councils will have to find £4.3 billion just to manage care services at the current levels. Furthermore, estimates that were produced for the Dilnot Commission suggest that even without reform, spending on social care will have to rise from £14.6 billion in 2010/11 to £23 billion by 2025/26. Local government has faced tough spending settlements over the last four years that have impacted dramatically on adult social care and its capacity to deliver. The prospects for third sector funding are fragile too. Combine this with the pace of demographic change, adult social care services will soon reach a critical point. This will have clear knock-on effects on and across the health care system unless we do things differently. Without investment in preventative and out of hospital services, even without the economic pressures, increases in the numbers of older people would mean more emergency admissions to hospital, delayed discharges and longer waits for treatment, as well as increased pressure on hospital accident and emergency departments. Care funding faces a deepening crisis which must be addressed. A better understanding of the reciprocal relationship between spending in health and social care is essential to ensure a holistic and integrated approach. 6 Purpose Document A Lancashire System Response to the Five Year Forward View The NHS “Five Year Forward View” NHS England recently published a “Five Year Forward View” that offered a route map for the proposed direction of travel for the health and care system over the next five years. The message that emerged from this Forward View was that we are at a crossroads. To secure the future that we all know is possible, we need to change radically, empower the public and work more closely with our partners. The purpose of the Five Year Forward View is to articulate why change is needed, what that change might look like and how we can achieve it. It envisages action on four fronts: • Action to tackle the root causes of ill health. The future of the NHS now depends on a radical upgrade in prevention and public health. The Forward View calls for hard-hitting action on obesity, alcohol abuse and other major health risks. • Action to meet the needs of a population that lives longer. This means breaking down the boundaries between family doctors and hospitals, between physical and mental health and between health and social care and it means getting better at dealing with the complexities associated with multiple long-term conditions. • Action to develop new models of care, greater flexibility and more investment in our workforce, technology and innovation. • A commitment to giving patients more control of their own care, including the option of combining health and social care, and new support for carers and third sector workers. The Forward View argues that if the NHS received flat real terms funding over the next five years, and made no further efficiency savings, then growing demand for healthcare would lead to a national NHS shortfall of £30bn a year by 2020/21. (The Lancashire share of this shortfall would be in the order of £830m.3) The Forward View says that to sustain a comprehensive, high-quality health and care system, action will be needed on all three fronts - demand, efficiency and funding. Much of the Forward View focuses on secondary care in hospitals, but it also recognises the importance of reforming primary care too. The challenges facing primary care include: • • • • • An increasing workload and falling income Poor career structures and problems with workforce recruitment and retention Under-utilised skills and a lack of investment in education and training Lack of investment in infrastructure including premises The challenge of seven-day working The Forward View leads the move towards a different health and care system. It does not propose a one-size-fits-all plan but nor does it suggest the solution is to let a ‘thousand flowers bloom’. Rather it sets the framework for further detailed planning about how health and care needs to evolve over the next five years and it invites health communities across England to respond by developing their own thinking. It represents a clear consensus that has developed between NHS England, Monitor, Health Education England, the NHS Trust Development Authority, Public Health England and the Care Quality Commission. It is the first time the NHS has set out a clear sense of direction for the way services need to change and improve. 7 Healthier Lancashire Programme An emerging consensus within Lancashire This national consensus is now being echoed across Lancashire. The Lancashire health community comprises eight Clinical Commissioning Groups (CCGs), more than 200 GP practices, five acute NHS hospital Trusts, a health and wellbeing Trust and a single specialty learning disability Trust. Social care is provided by Lancashire County Council and the two unitary authorities of Blackburn with Darwen and Blackpool. Additionally there is an active third sector supporting health and social care. Within this community there is a growing sense of common purpose and a growing sense of urgency around the need for change. Many of the themes in the Forward View have resonance in Lancashire too. For example, just over a decade ago the Derek Wanless health review warned that unless we took prevention seriously we would be faced with a sharply rising burden of avoidable illness. That warning was not heeded, the rising burden is upon us and the need for a radical upgrade in prevention and public health is now urgent. A priority for England AND for Lancashire. The Healthier Lancashire programme aims to significantly improve health and social care outcomes for the people of Lancashire and to radically shift the way in which health and social care services are delivered. The Leadership Forum started to develop a vision and a series of principles, which were refined at the summit in November. This means that we are able to put forward a clear vision… “All Lancashire people are united around a common cause; one that stops people from being patients” 8 ‘ The age of the passive patient is passing. The NHS of the future will be one of personal power and personal engagement. The time has come for us to encourage active citizen partnership in which people take greater control over - and assume greater responsibility for - their own health and care. Our aim should be nothing less than to stop people being patients before they absolutely need to be and to support them appropriately when they are. Purpose Document A Lancashire System Response to the Five Year Forward View When people need health or social care they will be treated as individuals, as equal partners in their care and will receive the best care possible. The programme is guided by some key objectives: • To set out a clear direction of travel for the health and care system in Lancashire as the Five Year Forward View has across England • To achieve fundamental and measurable improvements in health outcomes • To reduce health inequalities in Lancashire • To achieve parity of esteem for mental health and physical health • To ensure greater focus on health prevention, early intervention and self-care • To ensure change is supported by a clear evidence base or an evaluation structure where evidence is not available • To remove organisational or professional boundaries that get in the way of progress • To make maximum use of new technology. If we fail to address these objectives, if we do not embrace radical change, health outcomes in Lancashire will simply get worse, the quality of care will decline, individual services will fail, costs will rise and patient satisfaction will plummet. Lancashire - demographics and geography Lancashire is a fusion of urban and rural environments, stretching from the sea to the Pennines and includes two cities and several large towns. It is a diverse area with some of the most deprived communities in England and a few of the more affluent. This social and economic diversity is reflected in local health outcomes. The people of Lancashire are not as healthy as they should be. Life expectancy is eighteen months shorter than in the rest of the country, the prevalence of heart failure, asthma and depression are all higher than average and there are wide health inequalities both within Lancashire itself and between Lancashire and the rest of the country. Yet Lancashire is also a place of invention and innovation. It was here in the late 18th century that the industrial revolution took shape. The transition from hand production to mechanised manufacturing foreshadowed dramatic improvements in efficiency and productivity. It marked a major turning point in world history that eventually led to sustained improvements in the living standards of ordinary people. Today we need a new revolution - a revolution in health and social care that delivers similar efficiencies and improvements in standards. If we embrace this idea as our common cause we can inspire radical, unrecognisable change with Lancashire once again leading the way. 9 Healthier Lancashire Programme The strategic challenge Lancashire faces many of the same health and care challenges that other parts of England face, but it also has some unique challenges of its own. • People are living longer - typically with multiple long-term conditions (LTCs) that are expensive to manage. Lancashire has 24,000 more people with three or more LTCs than the national average. • The present health and care system is not designed to meet current needs. It is a complex system where despite the best intentions of professionals, patients can experience delays and frustration as they are handed between services, often without their records being available. • Lancashire faces significant variations in health outcomes, many of which are worse than those in other parts of England. • We face growing public demand for health and care services and growing public expectation that we will provide them effectively but the evidence suggests that the public – and indeed the staff delivering these core services – have little faith in our ability to deliver well. Ignoring these challenges is not an option. The moment of opportunity We will only address these challenges successfully if we seize this moment of opportunity to make strategic changes. We need to: • Encourage people to take their health seriously and assume greater responsibility for their own good health • Develop robust integrated care services across Lancashire that reduce the reliance on acute hospital-based services • Create a multi-skilled, flexible and responsive workforce • Enhance the role of the third sector to support mainstream services • Establish joint system leadership across Lancashire’s entire health and social care environment. The organisations that comprise the health and social care system in Lancashire can only address the challenges effectively if they address them together. Success requires a whole system approach. Nobody can fix this alone. The time has come for us to look beyond the interests of our individual organisations and towards the future development of the whole health and care economy in Lancashire, building on what is already working well. At the summit in November 2014 at Turf Moor, the views of many health and social care stakeholders were canvassed. The tone of this document is largely drawn from this event, and the proposals contained build on the original discussions of the Leadership Forum and conversations with key stakeholders. It has been co-created, co-designed and co-produced. This is a principle which will remain central throughout the Healthier Lancashire Programme. 10 Purpose Document A Lancashire System Response to the Five Year Forward View Some clear themes emerged: We must work together • Health and social care organisations need to offer leadership through an unprecedented collaboration - a whole system approach - involving people and organisations to define a new way of working. • We must create a confederation to break open silos and ensure Lancashire gets what it needs, through sharing best practice. • We must put aside our territorial ambitions and look beyond the ‘organisational’ towards the individual. We need not just a campaign but a social movement • It was clear that stakeholders believed that only a “common cause” campaign with clear and measurable objectives would deliver the right results for Lancashire. • However, even that wasn’t enough on its own. There was a feeling that this campaign needed to go further and become an all-embracing social movement that is value-based and commitment-led and to which everybody could contribute and from which everybody could benefit. Change should be revolutionary rather than evolutionary • The time has come for bold, brave, radical action. We need to challenge how things stand and shout loudly where necessary. • It is time to embrace the idea of becoming a rebel with a cause. It is time for the active and responsible person • To benefit from a fair and sustainable society - in which everyone has an improved chance of a longer, independent life - we all have responsibilities to participate more in our own health and wellbeing. It is all about keeping people fit and healthy for longer. • Our common cause should be to create a fair and sustainable society that stops people from being patients sooner than they really need to. The strategic challenges outlined can only be successfully addressed by having a firm-rooted understanding of the current health and care system in Lancashire. The following section, ‘Where we are starting from’, sets out to inform strategic change and seize this moment of opportunity. 11 Healthier Lancashire Programme HS Lancashire - brochure.qxp_Layout 1 19/12/2014 14:57 Page 10 Where we are starting The Evidencefrom Base Healthier Lancashire Programme One of the key principles of the Healthier Lancashire programme is that change should be supported by a clear evidence base. With this in mind, the Healthier Lancashire team commissioned a major piece of work to establish a “single truth” fact base about health and care in Lancashire. In summary, this work indicates the following: One of the key principles of the Healthier Lancashire programme is that change should be supported by a clear evidence base. With this in mind, the Healthier Lancashire team commissioned a major piece of work to establish a “single truth” fact base about health and care in Lancashire. Lancashire has an ageing population… In summary, this work indicates the following: People are living longer4. While this is good news, it also presents a number of challenges. Compared to the Lancashire has a higher proportion of people in all age Lancashire has anEngland ageingaverage, population… bands above 50 years old.5 And by 2021, there will be 42,000 more over-70s in Lancashire.6 Between 2014 and 2021, all eight of Lancashire’s CCGs will see growth of at least 13% in People are living longer1. While this is good news, it also presents a number of challenges. Compared their populations aged 70 or over.7 to the England average, Lancashire has a higher proportion of people in all age bands above 50 years old.2 And by 2021, there will be 42,000 more over-70s in Lancashire.3 Between 2014 and 2021, all 8 eight of Lancashire’s CCGs by willage seeband growth of at least 13% in their populations aged 70 or over.4 Proportion of population Proportion of population by age band5 Proportion of Population (%) 13 12 14% 13% 14 12% 13% 12% 11% 12% 12% 13% 12% 12% 12% 12% 11% 11 10% 10 9% 9 8 7 6 5% 6% 5 Lancashire 4 England 3 0-9 10 - 19 20-29 30-39 40-49 50-59 60-69 70-79 80+ L hire Age Bands With two thirds of hospital patients over retirement age, NHS England’s chief executive Simon Stevens has highlighted the ageing population as the greatest challenge facing the NHS. In line with this, residents of Lancashire aged between 81 and 90 use double the resources of a 51 to 60 year old. Furthermore, just 3% of the Lancashire’s population accounts for a disproportionately high percentage of hospital care spending (43%).6 12 Purpose Document A Lancashire System Response to the Five Year Forward View With two thirds of hospital patients over retirement age, NHS England’s chief executive Simon Stevens has Ithighlighted the ageing is guided by some keypopulation objectives: as the greatest challenge facing the health and care system. • To set out a clear direction of travel for the NHS in Lancashire as the of Lancashire aged has between 81NHS andacross 90 useEngland double the resources In line with this, residents Five Year Forward View for the of a 51 to 60 year old. Furthermore, just 3% of Lancashire’s population accounts for a • To achieve fundamental and measurable improvements in health 9 disproportionately high percentage of hospital care spending (43%). outcomes. • To reduce health inequalities in Lancashire • To ensure greater focus on health prevention, early intervention and self-care • To ensure change is supported by a clear evidence base or an evaluation structure where evidence is not available • To remove organisational or professional boundaries that get in the way of progress • To make maximum use of new technology Residents in Lancashire are less healthy than the national average… If we fail to address these objectives, if we do not embrace radical A priority must be to get better at preventing disease. Lancashire’s heart failure, asthma and change, health outcomes in Lancashire 10 will simply get worse, the quality depression rates are all in the highest quintile in England. of care will decline, individual services will fail, costs will rise and patient satisfaction will plummet. While the overall burden of disease is only expected to increase in the future, the scale of this challenge is uncertain. If recent trends continue, however, the number of people with diabetes will almost double to 175,000 by 2021/22.11 Similarly, the prevalence of cancer in Lancashire will more than double between now and 2021/22, up from 39,000 cases to 89,00012 cases and obesity will affect 275,000 people in Lancashire by 2021/22 (up by more than 70% compared with today).13 In addition, every CCG in Lancashire is already at or above the England average for prevalence of stroke14 and heart failure.15 Many Lancashire people have three or more longterm health conditions (LTCs)… While people in Lancashire are living longer, they are often living with a number of LTCs such as diabetes, heart disease and kidney disease, which impacts their quality of life and the number of ‘healthy’ life years they can expect to enjoy.16 Nationally, treatment and care for people with LTCs is estimated to absorb around £7 in every £10 of total health and social care spending.17 Lancashire has 20% more people (24,000 patients in total) with three or more LTCs compared with the England average. Currently, over 80% of hospital spending in Lancashire is expended on less than 15% of Lancashire’s population and this group includes the vast majority of people with LTCs. Efforts must be focused on providing better health and social care for those with multiple health conditions, as these patients also have a higher than average incidence of mental health problems (over 6% compared with just over 5% nationally)18 and they consider themselves to be poorly supported by the health and care system.19 People with multiple LTCs must be managed differently. Patients could and should be more involved in their own care, and better self-management would mean fewer hospital visits and lower costs to the health and care system in Lancashire. 13 Healthier Lancashire Programme Lancashire residents are also more likely to die early… Andlife Lancashire are more likely to die early… expectancyresidents of the average resident of Lancashire has increased by one year over the The last four years. However, this rate of increase has mirrored the national picture, meaning that the average English resident can expect to live 18 months longer than the average The average English resident can expect to live 18 months longer than the average resident of resident of Lancashire.20 Lancashire. 21 Life - years Lifeexpectancy expectancy - years18 Chorley and South Ribble CCG 86 Greater Preston CCG 84 Life Expectancy 82 80 West Lancs CCG Fylde and Wyre CCG Blackburn with Darwen Lancs North CCG CCG East Lancs CCG England average: 81.0 Blackpool CCG Lancashire average: 79.5 78 76 CCGs 74 The population populationcovered coveredbybyNHS NHS England’s Lancashire Area Team ranks out 25 area teams for The England’s Lancashire Area Team ranks 23rd23rd out of 25of area teams for under-75 mortality with most of Lancashire’s CCGs significantly above the England under-75 mortality with most of Lancashire’s CCGs significantly above the England average for under22 average for under-75 This is particularly parts ofwith some CCGs falling 19 75 mortality. This ismortality. particularly pronounced in pronounced certain partsinofcertain Lancashire, Lancashire, with some CCGs falling into the worst-performing 10% nationally for under-75 into the worst-performing 10% nationally for under-75 mortality20. 23 mortality . Preventing would significantly reduce premature death rates. The The majority of Preventing disease diseaseininthe thefirst firstplace place would significantly reduce premature death rates. majority of deaths from the major diseases, such as cancer, are related to lifestyle factors deaths from the major diseases, such as cancer, are related to lifestyle factors such as smoking, alcohol, such as smoking, alcohol, lack of21exercise and poor diet.24 This demands a radical upgrade in lack ofhealth exercise and poor This demands radical upgrade in public health services with a public services with adiet. heightened focus on a prevention. heightened focus on prevention. 14 Purpose Document A Lancashire System Response to the Five Year Forward View There are significant health inequalities within There are significant health inequalities within Lancashire… Lancashire… 22 The Health Health and and Social Social Care CareAct Act2012 2012recognised recognisedthe theimportance importance tackling health inequalities. The ofof tackling health 25 as well as across England, we need to take action to reduce both inequality of access In Lancashire, inequalities. In Lancashire, as well as across England, we need to take action to reduce both inequality of access and inequality outcome. Health inequalities most and and inequality of outcome. Healthofinequalities between the most between and leastthe deprived 20% of peop least deprived 20% of people in Lancashire have widened or remained static for a number of inequ Lancashire have widened or remained static for a number of diseases. As an example, health diseases. As an example, health inequality for diabetes sufferers increased significantly for diabetes sufferers increased significantly between 2009 and 2013.23 between 2009 and 2013.26 As well well as as faring faring poorly poorly on on the the national national scale, scale,there thereare arewide widevariations variationsinindisease diseaseprevalence prevalence within As within Lancashire too. The residents of one Lancashire CCG have among the highest 10%for of the Lancashire too. One Lancashire CCG is among the worst 10% of CCGs in the country prevalence rates in the country for the prevalence of 15 out of 22 major diseases while the prevalence of 15 out of 22 major diseases while another is not ranked among the worst2710% for a residents of another are not ranked among the worst 10% for any of the major diseases. 24 of the major diseases. The Marmot Review recognised that there is a social gradient in health – the lower a 28 The Marmot recognised that a social gradient in health –stem the lower a person’s socia person’s socialReview position, the worse his there or herishealth. Health inequalities from more 25 than just differences in income – education, geography, and gender can all play a role. position, the worse his or her health. Health inequalities stem from more than just differences in income – education, geography, and gender can all play a role. Comparisons between the most and least deprived 20% of people in Lancashire reveal massive health inequalities. For example, people in the most deprived quintile are over seven Comparisons between most andfrom leastdiabetes deprivedthan 20%those of people Lancashire reveal massive he times more likely to die the prematurely in theinleast deprived quintile. For all nine diseases highlighted in in the graph people in Lancashire at thetimes lowermore end likely to inequalities. For example, people the mostbelow, deprived quintile are over seven of the deprivation scale are than at least twice as likely die prematurely the prematurely from diabetes those in the least to deprived quintile. as Forpeople all nineatdiseases highlighte 29 opposite end of the deprivation scale. the graph below, people in Lancashire at the lower end of the deprivation scale are at least twice a likely to die prematurely as people at the opposite end of the deprivation scale.26 Size of health inequality gap within Lancashire – premature mortality30 Size of health inequality gap within Lancashire – premature mortality27 Inequality ratio between most and least deprived quintiles 7.5 7.18 7.0 6.5 6.0 5.5 5.0 4.65 4.5 4.0 3.5 3.48 2.98 3.0 3.07 2.59 2.5 2.33 2.49 2.11 2.0 1.5 1.0 0.5 0.0 Diabetes Respiratory disease COPD Digestive disease Chronic liver Lung cancer Circulatory disease disease CHD Stroke Page 15 Healthier Lancashire Programme Health services struggle to meet current performance targets… Services in Lancashire do not compare well nationally when it comes to meeting performance targets. Our hospitals are under increasing strain and are not able to focus on more complicated cases where their expertise is really needed. In the recent past, some of our hospitals have been identified by Keogh31 for review, and are working hard to improve their standards in the face of mounting pressures. Across England there is an increasing demand that the health and care system provides services seven days a week like many other industries. The lower level of service provision at the weekend means patients are more likely to die in hospital if they are admitted at the weekend and this problem is particularly acute in Lancashire. For example, at one Lancashire acute Trust the mortality rate is 23% higher than expected for weekend emergency admissions.32 It is not just secondary care that’s failing to meet performance targets. Seven of Lancashire’s eight CCGs have higher than average unplanned admissions for conditions that should normally be managed in a primary care setting.33 In addition, some Lancashire residents with LTCs are not adequately supported to remain independent because services are not available in the community and as a result they are being admitted into hospital. Patient experience is variable… A combination of financial and demographic pressures means our health and social care services are under greater pressure. Therefore, despite the shared commitment and dedication of our health service staff, we know that our hospitals vary in the quality of care they provide. Our residents’ experience of hospital services often lags behind expectations. We know, for example, that more than half of acute and specialist Trusts in Lancashire fall below the NHS average score for inpatient satisfaction.34 For outpatients, the picture is similarly bleak. One of our acute Trusts is in the bottom quintile of Trusts in England for outpatients in terms of patient satisfaction, while the other Lancashire Trusts fall in the middle of the pack nationally.35 Patient satisfaction with inpatient services is at best average but mostly below average and in two cases well below average.31 We want the public to be at the heart of everything we do – but too often their experience of health and social care services do not reflect that aim. We have a lot to do to make improvements in the coordination of patient-centred care to provide a seamless service, as well as assessing the compelling arguments for introducing seven day services. If we work together, we can increase the number of people having a positive experience of health and social care. 16 Purpose Document A Lancashire System Response to the Five Year Forward View Staff satisfaction is deteriorating Staff satisfaction is deteriorating It is not only our patients who are dissatisfied. NHS staff in Lancashire are also generally less It issatisfied not onlythan our they patients who dissatisfied. NHSstaff staffare in Lancashire are also generally less satis should be,are reflecting that while highly motivated to provide compassionate care,Three they are concerned about staffing levels, workloadpoorly pressures and recommend than they should be. of our hospital Trusts perform particularly on staff compromises to the quality of care they deliver. Three of our hospital Trusts perform 35 as a place to receive care. 37 particularly poorly on staff recommendation as a place to receive care. Staff at all of of ourour Trusts are less to aafriend friendororrelative relative than Staff at all Trusts are lesslikely likelytotorecommend recommend their their organisation organisation to 36 member.38 In 2010, four out of our five Trusts were above average than the NHS staff average NHSaverage staff member. In 2010, four out of our five Trusts were above average but by 2013 39 by 2013 all five were fivebut were below average.37 below average. The graph below shows that while generally NHS staff across England are becoming more Thelikely graph showstheir thatown while generally NHS staff across England are becoming to below recommend trust to friends and family, in Lancashire NHS staff are more likely to generally becoming likely to recommend theirinown Trust.40 NHS staff are generally becoming recommend their own less trust to friends and family, Lancashire likely to recommend their own Trust.38 Staff satisfaction with Trust as a place to receive care41 Staff satisfaction with Trust as a place to receive care39 68 70 64 65 60 55 64 60 54 57 66 62 62 56 51 50 59 51 47 Score (%) 45 40 35 30 25 England 2013 Percentile Lancashire East Lancs Lancs Teaching Morecambe Bay Blackpool 74% 89% 51% 82% 56% Southport & Ormskirk 92% And we face big workforce challenges… Recruiting and retaining medical, nursing and specialist staff poses a significant problem as does t employment of significant numbers of agency staff. In Lancashire, medical and dental staff turno exceeds the England average.40 As ever, there is a wide variation within Lancashire – with one of t hospitals’ turnover rate for medical and dental staff being in the highest 10% nationally.41 As a result of workforce shortages across the North West, there is a need to increase the number o in training and practice to ensure that the supply and demand gap is closed. A further challenge is we simply do not have enough medical and dental staff for the number of patients requiring treatm 17 Pag Healthier Lancashire Programme There are also big workforce challenges… Recruiting and retaining medical, nursing and specialist staff poses a significant problem, particularly in Emergency Medicine and Accident and Emergency Departments, as well as specialties of growing importance, such as Clinical and Interventional Radiology.42 The shortterm fix to these issues is to employ significant numbers of agency staff, which is an unsustainable solution. In Lancashire, medical and dental staff turnover exceeds the England average.43 As ever, there is a wide variation within Lancashire – with one of the hospitals’ turnover rate for medical and dental staff being in the highest 10% nationally.44 As a result of workforce shortages across the North West, there is a need to increase the number of GPs in training and practice to ensure that the supply and demand gap is closed. A further challenge is that we simply do not have enough medical and dental staff for the number of patients requiring treatment. While demand for health and social care services is growing… The demand for health and social care services in Lancashire is growing as the population ages and as people with ill health require more care. It is difficult to meet this increased demand because adult social care, community services and hospitals do not work together as well as they could. In the past three years, we have seen a 2.7% increase in overall hospital activity across Lancashire.45 Almost two-thirds of under-five year olds in Lancashire visited A&E last year alone, with 135 children visiting A&E more frequently than every other month. The very fact that parents feel the need to take children to A&E rather than to use their local GP service suggests that health services are not working in the way they should be, with people confused about which service to use and understandably choosing to go to the service that they know is available, even if they have to wait. Admissions to A&E vary widely across Lancashire. While one of the Lancashire CCGs has one of the highest emergency admission rates in the country for acute conditions that should not usually require hospital admission, another is significantly below the national average.46 Breaking down the barriers between different services is crucial if we are to improve both quality and efficiency of care, and to ensure a collaborative one-system approach. Our aim should be to give individuals the care and support they require in the most appropriate and efficient settings and to ensure a truly integrated service. 18 Purpose Document A Lancashire System Response to the Five Year Forward View Social care has challenges too… Social care services also face significant challenges, with the proportion of temporary staff being almost double the English average.47 In two of Lancashire’s three local authority areas, the vacancy rate is also higher than the England average. In fact, Lancashire’s social care vacancy rates have grown by 155% in the past three years, whereas they have grown less than three times as fast in England over the same time period.48 The third sector is not adequately financed to fill the gaps… There is a clear eagerness from the third sector in Lancashire to build on the work it already does and to do more through direct support services to help people to lead healthier lives, especially people with LTCs. It is also clear, however, that many third sector organisations are experiencing severe financial pressures and even continuing to fulfill their present functions is a challenge let alone expanding to do more, as detailed in the Five Year Forward View. Healthier Lancashire recognises the added social value the third sector brings and will work with the third sector, with local authorities and with commissioners to ensure that relationships are as effective as possible and that contracts are as flexible as they can be. 19 Healthier Lancashire Programme Creating a system wide programme The previous sections have detailed the need for a social movement to create a revolution that will lead to a radically different and better health and care system, but social movements don’t happen by themselves. They need structure, strong direction and leadership. To ensure success, an unprecedented collaboration, whole system approach is needed, to define a new and better future for the delivery of health and care. The emerging consensus is that the changes should include: • • • • All of Lancashire All providers All services All of the population It was evident at the recent Healthier Lancashire stakeholder event that a clear campaign with measurable objectives is needed to deliver the right results for Lancashire. Such a campaign would need to be preceded by the development of a Strategic Plan. 20 Purpose Document A Lancashire System Response to the Five Year Forward View Why a Strategic Plan? Other large scale change programmes including North-West London, Healthier Together in Greater Manchester, have found that the use of a Strategic Plan is essential to improve the planning and execution of the activities to successfully deliver the agreed outcomes. Strategic Plans are particularly useful in situations where: • There are a large number of disparate stakeholders involved • There is a need to show how a programme relates to the needs of each participating public sector partner • The system and its ambition is novel, risky and complex • The parameters of the programme are ill-defined, particularly the objectives and scope • There is a need to allow key stakeholders an early opportunity to influence the direction of programmes, avoiding abortive effort, and securing better value for money from the considerable sums of money which are sometimes spent on ill-specified programmes. • If the Strategic Plan is properly implemented it will lead to better decision-making and quicker decisions. What is a Strategic Plan? The Strategic Plan should be viewed as a scoping and planning document, designed to: • Establish the strategic context and need for the programme • Develop a financial model that can be used to make the economic case for change across Lancashire • Identify key dependencies between the programme and other developments • Identify the view of main stakeholders and gatekeepers and the position of potential public sector partners and other prospective partners • Identify a wide range of viable options for meeting the care model objectives • Appraise the relative efficacy of the options and their affordability and, where feasible, identify a short-list for more rigorous assessment at the Design Phase • Identify the critical success factors for developing and implementing the programme with emphasis on risk management and benefit realisation • Identify what further work needs to be undertaken to inform implementation. They are based upon widely accepted best practice programme management approaches that have been designed using learnings from a number of other large scale health and social care change programmes. These plans and structures have recently been tested at judicial review and were found to be robust. 21 Healthier Lancashire Programme A Strategic Plan for All Lancashire The Healthier Lancashire process plan and governance structure have been developed to include all health and social care services in Lancashire including children's services and mental health services. The proposed governance and programme arrangements for the Strategic Planning Phase are illustrated in the following diagram: 22 Purpose Document A Lancashire System Response to the Five Year Forward View Leadership Structures must be designed that create the space within which growth, innovation and action can flourish. Leaders must be recruited, trained and developed on a scale required to build the relationships, maintain the motivation, and carry out the strategising and action to achieve success. Therefore, the delivery of the Strategic Plan will require: The Programme Board to oversee the delivery of the Strategic Plan in line with the scope, aims and timescales agreed by the partner organisations. It will also receive inputs from Health and Wellbeing Boards, Health Overview and Scrutiny Committees and Healthwatch. This is also where Monitor, the NHS Trust Development Authority and the Care Quality Commission will input their views. The Programme Board will have an independent chair. The Care Quality Board to provide clinical and care professional leadership and assurance to the programme, ensuring the programme develops effective proposals for the delivery of quality standards and acting as ambassadors for the programme including representing the programme at public events. The Finance and Investment Group to ensure that the plans are within agreed budgets and will develop an estates strategy to support the delivery of any proposed care models. Organising The Programme Management Group will manage programme activities required for the delivery of the Strategic Plan in line with directions from the Programme Board, the Care Quality Board and the Finance and Investment Group. Actions and Activities The delivery of the Strategic Plan will require actions and activities to be driven across three complementary work streams: • Cultural Transformation • Care Components • Digital Technologies The cultural transformation work stream is an integral part of all aspects of the Healthier Lancashire work programme. It will involve developing the empowered person and an engaged population and workforce, utilising new technology to support self-care as well as making it easier for people to access support when they need it. It will facilitate change management, a greater role for the third sector and the development of effective collaborative leadership at the Lancashire level. It will support the work of the groups developing new care models. 23 Healthier Lancashire Programme The care professionals work stream will undertake the required activities to develop the possible options for the design phase. A range of care model components will be considered to ensure the ambition of providing a step change in care can be realised and deliver the improvements in quality, outcomes and accessibility that are required. The proposals will align closely with the Better Care Fund, QIPP programmes and other local projects, including the development of co-commissioning to support primary care development. It will also ensure alignment of its work with CIP programmes, NHS England, Monitor, TDA, CQC and other local projects. The digital technologies work stream will develop proposals for a digital health ecosystem that will underpin the work of the other groups and will be a key component of the drive for better health outcomes, improving the experience of care and service efficiency. As part of our strategy, we will be seeking to increase digital literacy, share digital records and build partnerships across industry, academia, and the third sector. The aim is to empower people to take more control of their health and wellbeing. Each of these groups will be developing plans and proposals within the agreed financial envelope. They will agree the enablers required for implementation including governance, cost implications, estates and capital requirements, workforce, contracting and IM&T. They will also engage with the public, patients, carers and staff to ensure understanding of, and sign-up to, the proposals. Healthier Lancashire Programme There are independencies between these three groups which will be managed through the Programme Management Group. Timetable It is proposed that the programme activities will be organised into five phases which will run Timetable from 2015 to 2020. These will overlap at certain points as detailed below. The Healthier programmeLancashire is currently organised into is five phases which runstages from 2015 to 2020 but which The Programme structured intowill five will overlap at certain points. Sep – May ‘15 Strategic Plan • Baseline SAF Model • Set up programme structure • Develop and signoff PID • Agrre resources • Recruit programme team • Write a Strategic Outline Case for Lancashire • Communications and Engagement Strategy Jun – Dec ‘15 Design • Develop case for change • Develop the Quality Standards • Develop the care model components • Develop options for service change • Equality Impact Assessment • Write business case document • Agree consultation plan and appoint resources • Stakeholder engagement and communication • External Assurance Process Jan – Mar ‘16 Mar – Jul ‘16 Implementation • Write business plans for prioritised care model components • Deliver public consultation if needed • Plan for post consultation • Stakeholder engagement and communications by law Delivery • Consider and respond to consultation feedback • Finalise proposal including additional work particularly on finance, workforce and implementation plans • Equality impact assessment • Stakeholder engagement and communications 24 Aug ’16 – Mar ‘20 Procurement, Contracting & Delivery • Detailed implementation plans • Service specifications • Commissioning intentions • Capital business cases (if required) • Service charge • Stakeholder engagement and communications Purpose Document A Lancashire System Response to the Five Year Forward View Key Deliverables, January – May 2015 The expected outcomes of the Strategic Plan are: • A clear definition of the problems across the whole system and the case for change. As well as ownership of a single overall position • Priorities for action – what we need to do as a whole system, a local system and individual organisations • Key tasks and the arrangements to make change happen • Collaborative leadership and consensus decision-making • Improved and mature relationships and value-based behaviours. Mobilising the Strategic Plan The Lancashire Leadership Forum has indicated its desire to act and behave differently in order to achieve radical change. Through the existing Director of Finance and Chief Financial Officer Group (Health and Local Authorities) which is chaired by NHS England, it has been agreed that specialist external expertise would ensure a robust Strategic Plan. The tender to deliver this piece of work will be undertaken through January 2015 with a completed delivery date of the end of May 2015. The key success factor for delivery of the Strategic Plan is that all members of the system work collaboratively at scale and pace. The specification for the Strategic Plan will involve ensuring the consolidation of existing information within the local health and social care economy into a Strategic Plan for the delivery of a new care system. A well run tender process with a detailed specification designed by all the health and social care stakeholder organisations of Healthier Lancashire will support local economies to assess and agree new care models in line with their ambitions to maximise the opportunities afforded by the Five Year Forward View. The proposed framework for the specification to ensure that the right expertise to enhance the development of the Strategic Plan between January and May 2015 will include: • The establishment of a baseline case – i.e. current service provision models, associated activity, costs and expenditure from all sectors. Including the interdependencies between local plans and schemes. • The use of current health and social care data to build a robust financial and economic model to include activity, workforce, estates, costs and expenditure. The use of financial metrics from both Commissioners and Providers. The outputs from current and recent successful Lancashire projects and measures demonstrating current levels of efficiencies. Other locally and nationally generated data to enable clinical and financial modelling. • The use of external benchmarking data in public/private sectors - organisations and examples to provide external perspectives and order of magnitude for cost savings. • The impact of utilising evidence-based and best standards of care e.g. Healthier Together Programme • Defining the “do nothing” scenario forecast and scale of the funding gap • The process testing of current proposed models within local systems and best practice alternatives for their impact on the baseline. This will include public health and needs assessment analysis, strategic modelling of activity and financial and human resource, utilisation of co-production methodology and testing through facilitated workshops. 25 Healthier Lancashire Programme • Undertaking scenario modelling and impact assessment on quality and affordability • Identifying assumptions and financial analysis - testing assumptions in respect of the opportunities they offer to improve the quality of care, the outcomes of care and the affordability of care over the next five years. • Identifying productivity opportunities and potential savings • Co-producing the benefits realisation plan • Developing further the strategic outcomes • Consider alternative funding and contractual agreement frameworks that will support sustainability of the health and care system (Prime Provider or Alliance Model for instance) • Establishing potential levels of transitional resource required, including the required dual running costs and outline realistic timescale for the milestone plan • Ensuring knowledge transfer for the development of the Programme Management Office required to support the delivery of a whole system integrated care approach. Underpinning Communication and Engagement Strategy for the Strategic Plan Best practice requires engagement of the public and workforce at all stages of the Programme, adopting the principles of co-production and co-design. The Strategic Plan requires a clear communications and engagement strategy against the same timeline. This will include the following: • • • • • • • Engagement with Health and Wellbeing Boards Summit 2 Engagement events in localities, involving the public, frontline staff and leaders MPs briefings Clinical engagement Development of social media platforms and launch of the brand Newsletters and other communications. 26 Purpose Document A Lancashire System Response to the Five Year Forward View Conclusion The Five Year Forward View acknowledges that while the values of the health and care system are unchanging, the service itself must change. We must move from the age of the passive patient to the age of the active, responsible and empowered person. Our aim must be nothing less than to stop people being patients before they absolutely need to and to support them appropriately when they do. The future is one of growing public expectations, emerging technologies and changing needs, all of which pose significant challenges and all of which demand change. There is a growing consensus in Lancashire that we cannot carry on as we are because: • We haven’t taken prevention as seriously as we should • We have poorer outcomes than we should • We are now faced with a sharply rising burden of avoidable illness and marked pressures on the health and care system. • We cannot ignore the context of the national financial challenges of meeting increasing demand with limited or zero growth. Lancashire Leadership Forum discussions with stakeholders reveal the same story that emerges from internal discussions with staff, stakeholders and health and care leaders: • • • • We must work together more effectively We need not just a campaign but a social movement Change should be revolutionary rather than evolutionary It is time for the active and responsible person This is what we must do if we are to tackle the unacceptable - indeed intolerable - liability of poor health outcomes that is apparent across Lancashire. Lancashire can no longer accept: • • • • • • Shorter life expectancy Higher rates of heart failure, asthma and depression Many more people with multiple long term conditions Shameful health inequalities Health services that struggle to meet performance targets Substandard patient satisfaction We need to act and act quickly. We need a programme approach that is designed to mobilise the necessary resources, recruit the right team of people to galvanise action, develop the case for change and the appropriate options, engage with all of our key stakeholders, develop final proposals and then ensure the delivery of radical system and service change. 27 Healthier Lancashire Programme Glossary of key terms BCF - the £3.8bn Better Care Fund (formerly the Integration Transformation Fund) was announced by the Government in the June 2013 spending round, to ensure a transformation in integrated health and social care. CCG - Clinical Commissioning Group, a local community group led by GPs and healthcare professionals responsible for commissioning healthcare services. CIP - a Cost Improvement Programme is the identification by an NHS Trust of schemes to increase efficiency/or reduce expenditure. CIPs can include both recurrent (year on year) and non-recurrent (one-off) savings. CQC - the Care Quality Commission is an executive non-departmental public body of the Department of Health. It was established in 2009 to regulate and inspect health and social care services in England. Dr Foster Hospital Guide - the Hospital Guide publishes data about acute hospital care across England. Health and Wellbeing Boards - established under the Health and Social Care Act 2012 as a forum where key leaders from the health and care system work together to improve the health and wellbeing of their local population and reduce health inequalities. Health and wellbeing board members collaborate to understand their local community's needs, agree priorities and encourage commissioners to work in a more joined-up way. HEE - Health Education England is the national leadership organisation for education, training and workforce development in the health sector. HSMR - the Hospital Standardised Mortality Ratio compares the expected rate of death in a hospital with the actual rate of death. Keogh Review – assessed patient safety and was carried out by Professor Sir Bruce Keogh in July 2013. This review was ordered by the Prime Minister in response to the Francis Inquiry into poor care at Mid Staffordshire Hospitals NHS Foundation Trust. LTCs - long-term health conditions cannot be cured but their symptoms and complications can usually be controlled with treatment. Examples are arthritis, asthma, diabetes, epilepsy and high blood pressure. Marmot Review - a report into health inequalities in England published in 2010 which proposed an evidence based strategy to address the social determinants of health, the conditions in which people are born, grow, live, work and age and which can lead to health inequalities. 28 Purpose Document A Lancashire System Response to the Five Year Forward View Monitor - an executive non-departmental public body of the Department of Health. It is the sector regulator for health services in England. The body was established in 2004 under the Health and Social Care (Community Health and Standards) Act 2003, which made it responsible for authorising, monitoring and regulating NHS foundation trusts. NHS Adult Inpatient Survey - this survey looks at the experiences of a sample of people who were admitted to an NHS hospital in a given year. NHS England - an executive non-departmental public body of the Department of Health. NHS England oversees the budget, planning, delivery and day-to-day operation of the commissioning side of the NHS in England as set out in the Health and Social Care Act 2012. NHS Five Year Forward View - was published on 23 October 2014 and sets out a vision for the future of the NHS. It was developed by the partner organisations that deliver and oversee health and care services including NHS England, Public Health England, Monitor, Health Education England, the Care Quality Commission and the NHS Trust Development Authority. Patient groups, clinicians and independent experts also provided their advice to create a collective view of how the health service needs to change over the next five years if it is to close the widening gaps in the health of the population, quality of care and the funding of services. NHS Outpatient Survey - a national survey of the views of patients' experiences which asked people about their most recent visit to an outpatient department. The survey included questions on waiting times, hospital facilities, seeing a doctor or other members of staff, tests and treatments and prescribed medications. NHS Staff Satisfaction Survey - an annual national survey of NHS staff. PHA - Public Health England is an executive agency of the Department of Health in the United Kingdom that began operating on 1 April 2013. Established under the Health and Social Care Act 201 it took on the role of the Health Protection Agency, the National Treatment Agency for Substance Misuse and a number of other health bodies. PROMS - Patient Reported Outcome Measures record health gain in patients undergoing hip replacement, knee replacement, varicose vein and groin hernia surgery in England, based on responses to questionnaires before and after surgery. QIPP - the Quality, Innovation, Productivity and Prevention programme is a large-scale programme developed by the Department of Health to drive forward quality improvements in NHS care, at the same time as making up to £20 billion of efficiency savings by 2014/15. Seven-day working - since 2010 there has been a growing movement towards more NHS services being available seven days a week. SHMI - the Summary Hospital-level Mortality Indicator is an indicator which reports on mortality at trust level across the NHS in England. The SHMI is the ratio between the actual number of patients who die following hospitalisation at the trust and the number that would be expected to die on the basis of average England figures, given the characteristics of the patients treated there. TDA - the NHS Trust Development Authority is responsible for providing leadership and support to the non-Foundation Trust sector of NHS providers. This includes 99 NHS Trusts, providing around £30bn of NHS funded care each year. Wanless Review - Securing our Future Health: Taking a Long-Term View was a report published in 2002 which assessed the long-term resource requirements for the health service in the UK. 29 Healthier Lancashire Programme References 1 https://www.gov.uk/government/publications/health-and-social-care-act-2012-fact-sheets 2 http://www.england.nhs.uk/ourwork/futurenhs/ 3 NHS England Lancashire Area Team Finance Team (not publically available). It is based on local allocations and may be subject to revision. Pg 284 Indexed Factbase, table 11.2 4 Select Committee on Public Service and Demographic Change - Report of Session 2012–13 - Ready for Ageing, March 2013 5 ONS data - http://www.ons.gov.uk/ons/guide-method/method-quality/specific/populationand-migration/pop-ests/index.html [Indexed Factbase p.17; section 2.2] 6 ONS data - http://www.ons.gov.uk/ons/guide-method/method-quality/specific/populationand-migration/pop-ests/index.html [Indexed Factbase p.15; section 2.1] 7 ONS data - http://www.ons.gov.uk/ons/guide-method/method-quality/specific/populationand-migration/pop-ests/index.html [Indexed Factbase p.15; section 2.1] 8 ONS data - http://www.ons.gov.uk/ons/guide-method/method-quality/specific/populationand-migration/pop-ests/index.html [Indexed Factbase p.17; section 2.1] 9 Secondary Uses Services (SUS) data provided by the CSU, which has also derived cost estimates [Indexed Factbase p.213; section 8.1] 10 Quality and Outcomes Framework (QOF); House of Care; CCG Outcomes Tool [Indexed Factbase p.37; section 3.1] 11 Quality and Outcomes Framework (QOF); House of Care; CCG Outcomes Tool [Indexed Factbase p.39; section 3.1] 12 Quality and Outcomes Framework (QOF); House of Care; CCG Outcomes Tool [Indexed Factbase p.39; section 3.1] 13 Quality and Outcomes Framework (QOF); House of Care; CCG Outcomes Tool [Indexed Factbase p.38; section 3.1] 14 QOF prevalence of disease by CCG, National General Practice Profiles & HSCIC [Indexed Factbase p.41; section 3.3] 15 CCG Outcomes Tool, 2012/13 [based on same QOF disease prevalence dataset] [Indexed Factbase p.42; section 3.5] 16 QOF prevalence of disease, National General Practice Profiles & HSCIC [Indexed Factbase p.54; Section 3.17]. Also see table 5.1 Healthy Life Expectancy: Years [Indexed Factbase p116] / ONS Data 17 Department of Health (2012). Report. Long-term conditions compendium of Information: 3rd edition 18 Quality and Outcomes Framework (QOF); House of Care; CCG Outcomes Tool [Indexed Factbase p.37; section 3.1] 19 CCG Outcomes Tool; House of Care [Indexed Factbase p.107; section 5.1] 20 ONS data [Indexed Factbase p.81; section 4.1] 30 Purpose Document A Lancashire System Response to the Five Year Forward View 21 ONS data [Indexed Factbase p.81; section 4.1] 22 ONS data [Indexed Factbase p.81; section 4.1] 23 Public Health England, Health Profiles 24 http://www.england.nhs.uk/wp-content/uploads/2013/07/nhs_belongs.pdf 25 http://www.legislation.gov.uk/ukpga/2012/7/contents/enacted 26 ONS data [Indexed Factbase p.81; section 4.1] 27 Quality and Outcomes Framework (QOF); House of Care; CCG Outcomes Tool [Indexed Factbase p.37; section 3.1] 28 http://www.instituteofhealthequity.org/projects/fair-society-healthy-lives-the-marmotreview 29 Public Health England [Indexed Factbase p.86; section 4.7] 30 Joint Strategic Needs Assessment (JSNA) Health inequalities in Lancashire, March 2014 [Indexed Factbase p.86; section 4.8] 31 http://www.nhs.uk/NHSEngland/bruce-keogh-review/Pages/Overview.aspx 32 HSCIC – http://www.hscic.gov.uk/ (current at 1st August 2014) [Indexed Factbase p.108; section 5.1] 33 CCG Outcomes Tool, 2012/13 data 34 NHS Adult Inpatient Survey 1st June 2013 – 31st August 2013; CCG Outcomes Tool, July 2014 [Indexed Factbase p.148; section 6.3] 35 NHS Outpatient Survey [Indexed Factbase p.145; section 6.1] 36 NHS Adult Inpatient Survey 1st June 2013 – 31st August 2013; CCG Outcomes Tool, July 2014 [Indexed Factbase p.148; section 6.3] 37 NHS Staff Satisfaction Survey [Indexed Factbase p.146; section 6.1] 38 NHS Staff Satisfaction Survey [Indexed Factbase p.146; section 6.1] 39 NHS Staff Satisfaction Survey [Indexed Factbase p.147; section 6.2] 40 NHS Staff Satisfaction Survey [Indexed Factbase p.147; section 6.2] 41 NHS Staff Satisfaction Survey [Indexed Factbase p.147; section 6.2] 42 Cumbria and Lancashire Local Workforce Education Group Workforce Plans 2014/15 – 2018/19, October 2014 [Indexed Factbase p.248] 43 CQC Intelligent Monitoring, 2014 [Indexed Factbase p.234; section 9.7] 44 CQC Intelligent Monitoring, 2013/14 [Indexed Factbase p.228; section 9.1] 45 SUS, Inpatient, Outpatient and A&E data [Indexed Factbase p.167; section 7.1] 46 SUS, Inpatient, Outpatient and A&E data, 2013/14 47 Skills for Care, August 2014 [Indexed Factbase p.254; section 10.1] 48 Skills for Care, August 2014 [Indexed Factbase p.254; section 10.1] 31 Healthier Lancashire Programme Member organisations of the Lancashire Leadership Forum Age UK Lancashire (on behalf of the Third Sector) Blackburn with Darwen CCG Blackburn with Darwen Council Blackpool CCG Blackpool Council Blackpool Teaching Hospitals NHS Foundation Trust Calderstones Partnership NHS Foundation Trust Chorley Council (on behalf of Lancashire District Councils) Chorley & South Ribble CCG East Lancashire CCG East Lancashire Hospitals Trust Fylde & Wyre CCG Greater Preston CCG Lancashire Care NHS Foundation Trust Lancashire County Council Lancashire North CCG Lancashire Teaching Hospitals NHS Foundation Trust NHS England North West Ambulance Service NHS Trust Progress Housing (on behalf of the Housing Federation) Public Health England Southport & Ormskirk Hospital NHS Trust University Hospitals of Morecambe Bay NHS Foundation Trust West Lancs CCG 32 GOVERNING BODY MEETING 14th January 2015 Date of Meeting Title of Report Governing Body Responsible Officer Summary/Purpose of Report Governing Body Action Agenda 17 Item No. Managing Conflicts of Interest – Revised Conflicts of Interest Policy Lead Dr Chris Clayton, Dr Malcolm Ridgway, Clinical Chief Officer Clinician Clinical Director for Quality and Effectiveness Lead Mr Iain Fletcher, Head of Manager Corporate Business The purpose of this report is to present the Clinical Commissioning Group’s (CCG) Governing Body with a revised Conflicts of Interest (CoI) Policy for approval. • • Note the contents of the report Review and approve the revised Conflicts of Interest Policy Please indicate the Committee(s)/Group(s) where the paper has been discussed/developed Primary Care Delivery Assurance Group Please note the following section must be completed in full Patient and Public Yes/Not (if yes, complete outcome) Engagement applicable Completed Equality Analysis was undertaken on the existing Equality Analysis Yes CCG policy and this will be reviewed to ensure no Completed additional impact due to the revisions made. If conflicts of interest are not managed effectively then there is Financial potential for challenge, which may have a financial implication. Implication(s) Yes – held on Governing Body Assurance Framework (Risk ID Risk(s) Identified C04.4) – “Failure to effectively manage conflicts of interest”) CCG Strategic Objectives supported by this paper 1. 2. 3. 4. 5. We will continuously improve the health and well-being of the population of Blackburn with Darwen. We will build successful partnerships which promote collaborative working and integrated service delivery. We will effectively engage patients and the public in decision making. We will co-commission and deliver continuous improvement in Primary Care Services and tackle inequalities. We will commission safe and effective services for the population of Blackburn with Darwen with integration at the heart of commissioning. Y Y Y Y Y CCG High Impact Changes supported by this paper 1. 2. 3. 4. 5. 6. 7. 8. 9. Delivering high quality Primary Care at scale and improving access. Self-Care and Early Intervention. Enhanced and Integrated Primary Care and Better Care Fund. Access to Re-ablement and Intermediate Care. Improved hospital discharge and reduced length of stay. Community based ambulatory care for specific conditions. Access to high quality Urgent and Emergency Care. Scheduled Care. Quality. Page 1 of 3 Y Managing Conflicts of Interest – Revised Conflicts of Interest Policy 1. Introduction 1.1 The purpose of this report is to present the Clinical Commissioning Group’s (CCG) Governing Body with a revised Conflicts of Interest (CoI) Policy for approval. 2. Background 2.1 As part of the CCG’s application to undertake delegated commissioning arrangements for Primary Medical Care Services, there is a requirement to submit details of how the CCG will manage conflicts of interest under the proposed delegated arrangements. 2.2 In December 2014, NHS England published statutory guidance setting out how CCGs should manage conflicts of interest with specific provisions in relation to cocommissioning primary medical care services. The guidance does not mandate what must be included in a CCG CoI policy, but states that non adherence must be explained. 2.3 The CCG’s existing policy has now been revised in accordance with the statutory guidance and has been submitted (as a draft document) to NHS England as part of the application process for delegated commissioning arrangements. 3.0 Overview of changes to existing arrangements for managing Conflicts of Interest 3.1 Attached at Appendix 1 is the revised CoI policy. The main amendments relate to the adherence of the regulations which govern the management of procurement decisions. The statutory guidance strengthens the wording within the revised policy to emphasise the importance managing potential conflicts of interest where a commissioner may also be a provider of services: “CCGs must not award a contract for the provision of NHS health care services, where conflicts, or potential conflicts, between the interests involved in commissioning such services and the interests involved in providing them affect, or appear to affect, the integrity of the award of that contract”. In addition, other changes to the policy based on the guidance, include the frequency of the review of the register of interests which is proposed to be undertaken quarterly, and the requirement to maintain and publish a register of procurement decisions which should be updated whenever a procurement decision is taken. The register must set out: 3.2 • • • The details of the decision Who was involved in making the decision (i.e. governing body or committee members and others with decision-making responsibility) A summary of any conflicts of interest in relation to the decision and how this was managed by the CCG To further support the management of conflicts of interest under the proposed delegated arrangements, the CCG has reviewed its governance processes and agreed that a subcommittee will be formed with delegated authority for decision making in support of primary care commissioning (medical services). The committee will have a lay and executive majority and will extend a standing invitation to a representative from the local Healthwatch organisation and the Health and Wellbeing Board. 3.3 Page 2 of 3 4. Conclusion 4.1 This report has provided the governing body with an update on the requirement to revise the CCG’s CoI policy based on the publication of statutory guidance and the proposed intention to undertake delegated arrangements for primary care commissioning (medical services) from 1st April 2015. 5. Recommendations 5.1 The Governing Body is requested to: • • Note the contents of the report Review and approve the revised Conflicts of Interest Policy Mrs Claire Moir Governance, Performance and Risk Manager January 2015 Page 3 of 3 Conflict of Interests Policy Author/s: Chief Finance Officer Governance, Performance and Risk Manager In Consultation with: NHS Blackburn with Darwen Clinical Commissioning Group Governing Body Formally ratified/approved by: CCG Governing Body Sphere of Activity: This policy spans all Clinical Commissioning Group activity Version Number: 3.0 Date of previous revisions: 1.0 All staff CCG website Health and Wellbeing Board Healthwatch Blackburn with Darwen Borough Council All Governing Body members, members of the CCG’s committees or sub-committees and its employees Distribution: Target Audience: POLICY STATEMENT / KEY OBJECTIVES This policy sets out how Blackburn with Darwen Clinical Commissioning Group (CCG) will manage conflicts of interest arising from the operation of the CCG’s business; it applies to the Governing Body members, members of the CCG’s committees or sub-committees and its employees, to ensure there can be confidence in the probity of commissioning decisions and the integrity of those involved with the work of the CCG. REFERENCES AND SUPPORTING DOCUMENTS • Managing Conflicts of Interest: Statutory Guidance for CCGs, December 2014 • Next steps towards primary care co-commissioning, November 2014 • Managing Conflicts of Interest: Guidance for Clinical Commissioning Groups, March 2013 • Code of Conduct: Managing Conflicts of Interest where GP practices are potential providers of CCG commissioned Services, October 2012 • Towards establishment: Creating responsive and accountable Clinical Commissioning Groups (and technical Appendix 1): Code of Conduct, February 2012 • Standards for Members of NHS Boards and Clinical Commissioning Group Governing Bodies in England, Professional Standards Authority, November 2012 Sponsoring Director: Chief Finance Officer Signature: Issue Date: January 2015 Page 1 of 18 Date Stage 1 of Equality Impact Assessment was carried out: 1st May 2013 Was a Stage 2 Equality Impact Assessment Carried out? n/a Date Stage 2 of Equality Impact Assessment was undertaken: n/a Date sent for ratification Date published on the Website Issue Date: January 2015 Page 2 of 18 CONTENTS PAGE 4 1. Introduction 1.1 Statement of Intent 4 2. Definitions 4 3. Statutory Requirements 5 4. Scope of Policy 5 5. Duties and Responsibilities 6 4.1 All CCG members 6 4.2 CCG Secretariat 8 6. Declaration of Interests 8 6.1 On Appointment 8 6.2 Quarterly 8 6.3 At Meetings 8 6.4 On Change of Role or Responsibility 9 6.5 On any other Change of Circumstance 9 7. Declarations of Interest in relation to procurement 7.1 Managing conflicts to protect the integrity of the decision-making process 9 10 8. Compliance 11 9. Review 11 Appendices 1 Declaration of conflict of interests for bidders/contractors template 13 2 Declaration of interests for members/employees template 15 Issue Date: January 2015 Page 3 of 18 1. Introduction The Governing Body of NHS Blackburn with Darwen Clinical Commissioning Group (CCG) has ultimate responsibility for all actions carried out by staff and committees throughout the CCG’s activities. This responsibility includes the stewardship of significant public resources and the commissioning of healthcare services to benefit the local community. The CCG recognises that it is not possible to avoid conflicts of interest: they are inevitable in many aspects of public life. By recognising where and how they arise and dealing with them appropriately, commissioners will be able to ensure proper governance, robust decision making and appropriate decisions about the use of public money 1.1 Statement of Intent The CCG is determined to ensure the organisation inspires confidence and trust amongst its patients, staff, partners, funders and suppliers by demonstrating integrity and avoiding any potential or real situations of undue bias or influence in the decision-making of the CCG. 2. Definitions A conflict of interest occurs where an individual’s ability to exercise judgement or act in one role is or could be impaired or otherwise influenced by his or her involvement in another role or relationship. The individual does not need to exploit his or her position or obtain an actual benefit, financial or otherwise. A potential for competing interests and/or a perception of wrongdoing, impaired judgement or undue influence can also be as detrimental as any of them occurring. As well as direct financial interests, conflicts can arise from an indirect financial interest (e.g. payment to a spouse) or a non-financial interest (e.g. kudos or reputation). Conflicts of loyalty may arise (e.g. in respect of an organisation of which the individual is a member or has an affiliation). Conflicts can arise from personal or professional relationships with others (e.g. where the role or interest of a family member, friend or acquaintance may influence an individual’s judgement or actions or could be perceived to do so. Depending on individual circumstances, these factors can all give rise to potential or actual conflicts of interest. For any individual involved in commissioning, a conflict of interest may, therefore, arise when their own judgement as an NHS commissioner could be, or be perceived to be, influenced and impaired by their own concerns and obligations as a healthcare or related provider, as a member of a particular peer, professional or special interest group, or as a friend or family member. For GPs involved in commissioning, an obvious example is the award of a new contract to a provider in which an individual GP has a financial stake. The underpinning principles for managing conflicts of interest within the CCG are to ensure that: • • • • The CCG is able to do business appropriately Conflicts of Interest are managed proactively not reactively The CCG and clinicians in commissioning roles demonstrate that they are acting fairly and transparently and in the best interests of their patients The CCG operates within the legal framework, but without being bound by overprescriptive rules that risk stifling innovation Issue Date: January 2015 Page 4 of 18 • • • The public, providers, Parliament and regulators have confidence in the probity, integrity and fairness of commissioners’ decisions The confidence and trust between patients and GP, in the recognition that individual commissioners want to behave ethically but may need support and training to understand when conflicts (whether actual or potential) may arise and how to manage them if they do A balanced and proportionate approach is maintained to safeguard clinically led commissioning, whilst ensuring objective investment decisions To support staff, and ensure the principles with the policy are implemented, the following definitions are offered: a “fundamental interest” would require the individual to withdraw from the meeting room completely, and take no part in the debate or the decision-making process. A “significant interest” would allow the individual to remain in the meeting, and to participate in the discussion, but to abstain from taking part in the decision-making process. 3. Statutory Requirements Section 14O of the National Health Service Act, 2006, inserted by section 25 of the 2012 Health and Social Care Act, sets out that each CCG must: • • • • • Maintain one or more registers of interest of: the members of the group, members of its governing body, members of its committees or sub-committees of its governing body, and its employees Publish or make arrangements to ensure that members of the public have access to these registers on request Make arrangements to ensure individuals declare any conflict or potential conflict in relation to a decision to be made by the group, and record them in registers as soon as they become aware of it, and within 28 days; and Make arrangements, set out in their constitution, for managing conflicts of interest, and potential conflicts of interest in such a way as to ensure that they do not and do not appear to affect the integrity of the CCG’s decision-making process Have regard to guidance published by NHS England and Monitor in relation to conflicts of interest The NHS (Procurement, Patient Choice and Competition) Regulations 2013 set out that commissioners: • Must not award a contract for the provision of NHS health care services where conflicts, or potential conflicts, between the interests of those involved in commissioning such services and the interests involved in those providing them affect, or appear to affect, the integrity of the award of that contract • Must keep a record of how it managed any such conflict in relation to NHS commissioning contracts it enters into. The CCG will ensure that details of all contracts awarded, including contract value, are published on the CCG’s website as soon as the contract is agreed. For the purpose of regulation 6 of the NHS procurement regulations (2013) an interest is defined as including an interest of the following: • A member of the commissioner organisation Issue Date: January 2015 Page 5 of 18 • • • A member of the governing body of the commissioner A member of its committees or sub-committees, or committees or sub-committees of its governing body; or An employee This is set out in detail in the CCGs Constitution (Part 8, Para 8.4 Transparency in Procuring Services). 4. Scope of Policy This policy applies to the Governing Body members, members of the CCG’s committees and sub-committees and all employees of NHS Blackburn with Darwen CCG. It will be the subject of review no later than 6 months after initial approval and annually thereafter. The CCG Governing Body members will be supplied with a copy of the policy on appointment by the Chair of the CCG, and will be available on the CCG’s website. The Governing Body has a legal obligation to act in the best interests of NHS Blackburn with Darwen CCG, and in accordance with the CCG’s constitution and terms of establishment created by the NHS England. 5. Duties and Responsibilities 5.1 All CCG Governing Body Members, Committee or Sub-Committee Members and Employees All CCG Governing Body members, committee or sub-committee members and employees are required to declare any relevant and material personal or business interests and any relevant and material personal or business interests of their spouse; civil partner; cohabitee; family member or any other relationship which may influence or may be perceived to influence their judgement. Examples of interests that will be deemed to be relevant and material include:- • • • • • • • • Roles and responsibilities held within member practices Directorships including non-executive directorships, held in private companies or PLCs Ownership or part-ownership of private companies, businesses or consultancies likely or possibly seeking to do business with the CCG Shareholdings (more than 5%) of companies in the field of health and social care A position of authority in an organisation (e.g. a charity or voluntary organisation) in the field of health and social care Any connection with a voluntary or other organisation contracting for NHS services Research funding/grants that may be received by the individual or any organisation in which they have an interest or role Any other role or relationship which the public could perceive would impair or otherwise influence the individual’s judgement or actions in their role within the CCG Where an individual changes role or responsibility within the CCG any change to the individual’s interest should be declared. Wherever an individual’s circumstances change in a way that affects the individual’s interests (e.g. where an individual takes on a new role outside of the CCG or sets up a new business or relationship), a further declaration should Issue Date: January 2015 Page 6 of 18 be made to reflect the change in circumstances. This could involve a conflict of interest ceasing to exist or a new one materialising. In the case of the Registered Nurse and the Secondary Care Consultant, if they become an employee or member (including shareholder) of, or a partner in/with: a) A person who is a provider of primary medical services for the purposes of Chapter A2 of the 2006 Act; or b) A body which provides any relevant service to a person for whom the CCG has responsibility they have a statutory interest which, on declaration, debars them from continuing as members of the CCG Governing Body. There are similar scenarios in the governing legislation which debar individuals from becoming, or continuing as, CCG Lay Members, or Governing Body members at all. If these scenarios occur, such as election to Parliament or to a Member role in a Local Authority, again the event and consequent declaration would debar the individual concerned from continuing as a Governing Body member. A waiver will apply in relation to the disability to participate in the proceedings of the CCG on account of a pecuniary interest. It will apply to: (i) A member of the Blackburn with Darwen Clinical Commissioning Group (“the CCG”) who is a healthcare professional, within the meaning of regulation 5(5) of the Regulations, and who is providing or performing, or assisting in the provision or performance, of– (a) services under the National Health Service Act 1977; or (b) services in connection with a pilot scheme under the National Health Service (Primary Care) Act 1997; (ii) Where the pecuniary interest of the member in the matter which is the subject of consideration at a meeting at which he is present:(a) arises by reason only of the member’s role as such a professional providing or performing, or assisting in the provision or performance of, those services to those persons; (b) has been declared by the relevant chair as an interest which cannot reasonably be regarded as an interest more substantial than that of the majority of other persons who:– (i) are members of the same profession as the member in question; (ii) are providing or performing, or assisting in the provision or performance of, such of those services as he provides or performs, or assists in the provision or performance of, for the benefit of persons for whom the CCG is responsible. Issue Date: January 2015 Page 7 of 18 (iii) Conditions which apply to the waiver and the removal of having a pecuniary interest The removal is subject to the following conditions: (a) the member must disclose his interest as soon as practicable after the commencement of the meeting and this must be recorded in the minutes; (b) the relevant chair must consult the Clinical Chief Officer before making a declaration in relation to the member in question pursuant to paragraph 7.3.3 (2) (b) above, except where that member is the Clinical Chief Officer; In the case of a meeting of the CCG: 5.2 (a) the member may take part in the consideration or discussion of the matter which must be subjected to a vote and the outcome recorded; but (b) may not vote on any question with respect to it. CCG Secretariat The CCG secretariat, on behalf of the CCG Chair, will maintain a register of interests declared by the CCG Governing Body members, committee or sub-committee members and employees, together with the date that the interest was declared. The register of interests will be refreshed every three months and an annual check will be carried out to ensure the register is accurate and up to date. All interests declared will be published in the CCG’s Annual Report; the register will be made available upon request either by post or email, and can also be accessed from the CCG’s website. 6. Declarations of Interests 6.1 Pre and On Appointment Applicants for any appointment to the CCG or its Governing Body will be asked to declare relevant interests to ensure there is no conflict so significant that it would debar them from appointment. When an appointment is made, a formal declaration of interests should be made again and recorded. 6.2 Quarterly All interests should be confirmed on a quarterly basis to ensure that the information is accurate and up to date. 6.3 At Meetings At all meetings including external and public meetings, all individuals should declare any interest that they have in any agenda item before it is discussed or as soon as it becomes apparent. Even if the interest has already been declared in the Register of Interests, it should be declared in meetings where matters relating to that interest are discussed. Declarations of interest should then be recorded in the minutes. Issue Date: January 2015 Page 8 of 18 In the event of the committee having to decide upon a question in which an individual has an interest, all decisions will be made by vote, with a simple majority required. A quorum must be present for the discussion and decision; interested parties will not be counted when deciding whether the meeting meets quorum requirements. Interested governing body members must not vote on matters affecting their own interests, even where the use of the waiver has been approved by the Chair and used, they may however take part in the discussions but will be excluded from the decision. One of the lay members will undertake the role of Deputy Chair and they would take the Chair’s role for discussions and decisions involving a conflict of interest for the Chair. All decisions under a conflict of interest will be reported in the minutes of the meeting with the following information:• the nature and extent of the conflict • an outline of the discussion • the actions taken to manage the conflict • use of the waiver and reasons for its implementation. Where an individual benefits from the decision, this will be reported in the annual report and accounts, as a matter of best practice. All payments or benefits in kind to governing body members will be reported in the CCG’s accounts and annual report, with amounts for each governing body member listed for the year in question. Independent external mediation will be used where conflicts cannot be resolved through the usual procedures. The committee may consider that there are certain conflicts of interest that are so fundamental that the individual concerned should be excluded from the meeting or the relevant part of the meeting, during which related issues are discussed. The Chair will have responsibility for deciding whether there is a conflict and the course of action to be taken and all decisions recorded in the minutes. For certain conflicts, the decision will need to be made on a case-by-case basis and the final decision made by the Chair. Where the CCG Governing Body is required to make a decision where the majority of the GP members have a declared conflict, the following process will be invoked: a) The decision will be voted on by the remaining members who are not conflicted in respect of the single agenda item. To achieve quoracy in such a situation at least five of the following members (and any non-conflicted GP members) should be present at the beginning of the meeting: • Chair • Chief Operating Officer • Chief Finance Officer • Registered Nurse • Secondary Care Doctor • Lay members 6.4 On Changing Role or Responsibility Wherever an individual changes role or responsibility within the CCG or its Governing Body any change to the individual’s interests should be declared within 28 days of becoming known. 6.5 On any other Change of Circumstances Wherever an individual’s circumstances change in a way that affects the individual’s interests (e.g. where an individual takes on a role outside of the CCG or sets up a new business or relationship), a further declaration should be made to reflect the change in Issue Date: January 2015 Page 9 of 18 circumstances. This could involve a conflict of interest ceasing to exist or a new one materialising. 7. Declaration of Interests in relation to procurement Where a relevant and fundamental interest or position of influence exists in the context of the specification for, or award of, a contract the individual will be expected to: • Declare the interest; • Ensure that the interest is recorded in the register; • Withdraw from all discussion on the specification or award; • Not have a vote in relation to the specification or award. It is expected that all interests are declared at the outset of any procurement process if the individual intends to be a potential bidder in that process. Failure to do so could result in the procurement process being declared invalid and possible suspension of that individual from the CCG. Potential conflicts will vary to some degree depending on the way in which a service is being commissioned e.g. where a CCG is commissioning a service through Competitive Tender (i.e. seeking to identify the best provider or set of providers for a service) a conflict of interest may arise where GP practices or other providers in which the individual has an interest are amongst those bidding, or where the CCG is commissioning a service through Any Qualified Provider a conflict could arise where one or more GP practices (or other providers in which individuals have an interest) are amongst the qualified providers from whom patients can choose. Guidance within the GMC’s core guidance Good Medical Practice (2006) and reiterated in its document Conflicts of Interest (2008) indicates, in such cases, that: “You must act in your patients best interests when making referrals and when providing or arranging treatment of care. You must not ask for or accept any inducement, gift or hospitality which may affect or be seen to affect the way you prescribe, treat or refer patients. You must not offer such inducements to colleagues if you have financial or commercial interest in organisations providing healthcare or in pharmaceutical or other biomedical companies, these interests must not affect the way you prescribe for, treat or refer patients. If you have a financial or commercial interest in an organisation to which you plan to refer a patient for treatment or investigation, you must also tell the patient about your interest. When treating NHS patients you must also tell the healthcare provider.” The GMC also provides the following general guidance: “You may wish to note on the patient’s record when an unavoidable conflict of interest arises; and if you have a financial interest in an institution and are working under an NHS employers’ policy you should satisfy yourself, or seek other assurance from your employing or contracting body, that systems are in place to ensure transparency and to avoid, or minimise the effects of, conflicts interest. You must follow the procedures governing the schemes.” 7.1 Register of Procurement Decisions A register of procurement decisions will be maintained by the CCG which will include: Issue Date: January 2015 Page 10 of 18 • • • The details of the decision Who was involved in making the decision (i.e. governing body or committee members and others with decision-making responsibility) A summary of any conflicts of interest in relation to the decision and how this was managed by the CCG The register will be updated whenever a procurement decision is taken. In the interests of transparency, the register of interests and register of decisions will be made available via the CCG’s website or upon request to the CCG. Making evidence of deliberation on conflicts publicly available will provide assurance: • • • • 7.2 That the CCG is seeking and encouraging scrutiny of its decision-making process; To the Health and Wellbeing Board, local Healthwatch and the local community that the proposed service meets local needs and prioities; it will enable them to raise questions if they have concerns about the approach being taken; To the Audit Committee and where necessary, external auditors, that a robust process has been followed in deciding to commission the service, in selecting the appropriate procurement route and, in addressing potential conflicts; To NHS England in their role as assurers of the delegated commissioning arrangements Managing conflicts to protect the integrity of the decision-making process To support the CCG to deliver its statutory requirements the following features will need to be integral to the commissioning of all services. They will be particularly important at the key commissioning decision making points leading up to and after the actual procurement of services and in deciding whether to go out to procurement: • • • • • • • • Openness: ensuring early engagement with patients, the public and health and wellbeing boards in relation to proposed commissioning plans. Governing Body members will also be members of the Health and Wellbeing Board and ensure that plans are supportive of the Health and Wellbeing Strategy. The Governing Body also has an engagement plan which sets out how patients the public will be involved in the work of the CCG Transparency: a clearly documented approach to be taken at each stage of the commissioning cycle Responsive and best practice: commissioning intentions are based on local health needs and reflect evidence of best practice – securing “buy-in” from patients and clinicians to the clinical case for change Securing expert advice: ensure that plans take account advice from appropriate health and social care professionals e.g. through the clinical senate and networks; and draw on commissioning support e.g. for more formal consultations and for procurement processes Engaging with providers: early engagement with both incumbent and potential new providers over potential changes to the commissioned services for the local population through involving them in the re-development of care pathways Create clear and transparent commissioning specifications: that reflect the depth of engagement and set out the basis on which any contract will be awarded Follow proper procurement processes: and legal arrangements, including even handed approach to providers Ensure sound record-keeping, including an up to date register of interests: applying best practice in sound record-keeping, making appropriate information Issue Date: January 2015 Page 11 of 18 • 8. available and accessible, and maintaining a register of interest with a clear system for declaration of interests Dispute resolution: having systems for resolving disputes, clearly set out in advance Compliance Failure to comply with this policy will be addressed under the disciplinary processes of the CCG, or otherwise as set out in the CCGs Standing Orders for Members of the Governing Body. 9. Review The Governance, Performance and Risk Manager will ensure this document is reviewed in accordance with the Review Date. The policy will be reviewed earlier should the CCG become aware of changes in practice, changes to statutory requirements, revised professional or clinical standards and local / national directives that affect, or could potentially affect the policy. Issue Date: January 2015 Page 12 of 18 Appendix 1 Declaration of conflict of interests for bidders/contractors template NHS Blackburn with Darwen Clinical Commissioning Group Bidders/potential contractors/service providers declaration form: financial and other interests This form is required to be completed in accordance with the CCG’s Constitution, and s140 of the NHS Act 2006 (as amended by the Health and Social Care Act 2012) and the NHS (Procurement, Patient Choice and Competition) (No2) Regulations 2013 and related guidance Notes: • All potential bidders/contractors/service providers, including sub-contractors, members of a consortium, advisers or other associated parties (Relevant Organisation) are required to identify any potential conflicts of interest that could arise if the Relevant Organisation were to take part in any procurement process and/or provide services under, or otherwise enter into any contract with, the CCG, in circumstances where the CCG is jointly commissioning the service with, or acting under a delegation from, NHS England. If any assistance is required in order to complete this form, then the Relevant Organisation should contact the CCG for clarification. • The completed form should be sent to the Head of Corporate Business. • Any changes to interests declared either during the procurement process or during the term of any contract subsequently entered into by the Relevant Organisation and the CCG must notified to the CCG by completing a new declaration form and submitting it to the Head of Corporate Business • Relevant Organisations completing this declaration form must provide sufficient detail of each interest so that the CCG, NHS England and also a member of the public would be able to understand clearly the sort of financial or other interest the person concerned has and the circumstances in which a conflict of interest with the business or running of the CCG or NHS England (including the award of a contract) might arise. • If in doubt as to whether a conflict of interests could arise, a declaration of the interest should be made. Interests that must be declared (whether such interests are those of the Relevant Person themselves or of a family member, close friend or other acquaintance of the Relevant Person), include the following: • • the Relevant Organisation or any person employed or engaged by or otherwise connected with a Relevant Organisation (Relevant Person) has provided or is providing services or other work for the CCG or NHS England; a Relevant Organisation or Relevant Person is providing services or other work for any other potential bidder in respect of this project or procurement process; Issue Date: January 2015 Page 13 of 18 • the Relevant Organisation or any Relevant Person has any other connection with the CCG or NHS England, whether personal or professional, which the public could perceive may impair or otherwise influence the CCG’s or any of its members’ or employees’ judgements, decisions or actions. Declarations: Name of Relevant Organisation: Interests Type of Interest Details Provision of services or other work for the CCG or NHS England Provision of services or other work for any other potential bidder in respect of this project or procurement process Any other connection with the CCG or NHS England, whether personal or professional, which the public could perceive may impair or otherwise influence the CCG’s or any of its members’ or employees’ judgements, decisions or actions Name of Relevant Person [complete for all Relevant Persons] Interests Issue Date: January 2015 Page 14 of 18 Type of Interest Details Personal interest or that of a family member, close friend or other acquaintance? Provision of services or other work for the CCG or NHS England Provision of services or other work for any other potential bidder in respect of this project or procurement process Any other connection with the CCG or NHS England, whether personal or professional, which the public could perceive may impair or otherwise influence the CCG’s or any of its members’ or employees’ judgements, decisions or actions To the best of my knowledge and belief, the above information is complete and correct. I undertake to update as necessary the information. Signed: On behalf of: Date: Issue Date: January 2015 Page 15 of 18 Appendix 2 Declaration of interests for members/employees template NHS Blackburn with Darwen Clinical Commissioning Group Member/ employee/ governing body member/committee or sub-committee member (including committees and sub-committees of the governing body) [delete as appropriate] declaration form: financial and other interests This form is required to be completed in accordance with the CCG’s Constitution and section 14O of The National Health Service Act 2006, the NHS (Procurement, Patient Choice and Competition) regulations 2013 and the Substantive guidance on the Procurement, Patient Choice and Competition Regulations Notes: • • • • • • • • Each CCG must make arrangements to ensure that the persons mentioned above declare any interest which may lead to a conflict with the interests of the CCG and the public for whom they commission services in relation to a decision to be made by the CCG or which may affect or appear to affect the integrity of the award of any contract by the CCG. A declaration must be made of any interest likely to lead to a conflict or potential conflict as soon as the individual becomes aware of it, and within 28 days. If any assistance is required in order to complete this form, then the individual should contact the Head of Corporate Business, or the Governance, Performance and Risk Manager. The completed form should be sent by both email and signed hard copy to the Head of Corporate Business. Any changes to interests declared must also be registered within 28 days by completing and submitting a new declaration form. The register will be published on the CCG website at blackburnwithdarwenccg.nhs.uk Any individual – and in particular members and employees of the CCG must provide sufficient detail of the interest, and the potential for conflict with the interests of the CCG and the public for whom they commission services, to enable a lay person to understand the implications and why the interest needs to be registered. If there is any doubt as to whether or not a conflict of interests could arise, a declaration of the interest must be made. Interests that must be declared (whether such interests are those of the individual themselves or of a family member, close friend or other acquaintance of the individual) include: • roles and responsibilities held within member practices; • directorships, including non-executive directorships, held in private companies or PLCs; • ownership or part-ownership of private companies, businesses or consultancies likely or possibly seeking to do business with the CCG; Issue Date: January 2015 Page 16 of 18 • • • • • shareholdings (more than 5%) of companies in the field of health and social care; a position of authority in an organisation (e.g. charity or voluntary organisation) in the field of health and social care; any connection with a voluntary or other organisation (public or private) contracting for NHS services; research funding/grants that may be received by the individual or any organisation in which they have an interest or role; any other role or relationship which the public could perceive would impair or otherwise influence the individual’s judgment or actions in their role within the CCG. If there is any doubt as to whether or not an interest is relevant, a declaration of the interest must be made. Declaration: Name: Position within or relationship with, the CCG: Interests Type of Interest Details Personal interest or that of a family member, close friend or other acquaintance? Roles and responsibilities held within member practices Directorships, including nonexecutive directorships, held in private companies or PLCs Ownership or part ownership of private companies, businesses or consultancies likely or possibly seeking to do business with the CCG Issue Date: January 2015 Page 17 of 18 Shareholdings (more than 5%) of companies in the field of health and social care Positions of authority in an organisation (e.g. charity or voluntary organisation) in the field of health and social care Any connection with a voluntary or other organisation contracting for NHS services Research funding/grants that may be received by the individual or any organisation they have an interest or role in [Other specific interests?] Any other role or relationship which the public could perceive would impair or otherwise influence the individual’s judgment or actions in their role within the CCG. To the best of my knowledge and belief, the above information is complete and correct. I undertake to update as necessary the information provided and to review the accuracy of the information provided regularly and no longer than annually. I give my consent for the information to be used for the purposes described in the CCG’s Constitution and published accordingly. Signed: Date: Issue Date: January 2015 Page 18 of 18 Agenda Item 18 NHS BLACKBURN WITH DARWEN CLINICAL COMMISSIONING GROUP (CCG) GOVERNING BODY MEETING 14TH JANUARY 2015 Report Title: Lancashire Collaborative Commissioning Board Terms of Reference and Membership Written By: Mr Peter Tinson, Chief Operating Officer, Fylde and Wyre CCG and Mr Carl Ashworth, Strategic Locality Lead – Fylde & Wyre CCG, Midlands and Lancashire Commissioning Support Unit Presented By: Mr Roger Parr, Chief Finance Officer, Blackburn with Darwen CCG Purpose of the paper: The purpose of this paper is to present for approval the Terms of Reference and Membership (v6.0) of the Lancashire Collaborative Commissioning Board (CCB) for consideration and approval by the members of the CCGs’ Governing Bodies. Key Issues: Members are asked to receive the CCB Terms of Reference and Membership (v6.1) The Terms of Reference and Membership include the following: • Definition • Aim • Range of benefits • Principles • Responsibilities • Process for Programme Management • Management of Programme Change Control • Membership • Authority Accountability and Governance • Chair • Role of the Senior Responsible Officer • Frequency of Meetings • Agenda and Meetings • Quorum • Reporting Review • Overall CCB Process • Strategic Model • CCB Architecture • Responsibilities for Management of papers Actions Required by Collaborative Commissioning Board Members: Members are asked to consider and approve the CCB Terms of Reference and Membership (v6.1) CCB Terms of Reference and Membership 20 November 2014 Collaborative Commissioning Board Item 18 Terms of Reference and Membership (v6.1) 1 Definition Collaborative commissioning is the process whereby two or more commissioners work together in order to effectively commission some of the services for which they are responsible, but also to share risk safely, transfer skills and secure commissioning support. 2 Aim To collaboratively commission efficient and effective health care for Lancashire residents, where there is benefit from commissioning on a larger footprint. 3 Range of Benefits The expected benefits include:‐ Clinical Improvement • Consistent, evidence based pathway development • Effective and consistent performance management, clinical governance and risk management • Service integration Efficiency • Leverage with providers • Keeping transaction costs low • Sharing (potentially scarce) expertise and capacity Resilience and risk management • Managing financial risks • Managing regulatory and legal change • Managing extended absence of key staff • Improved risk management and intelligence systems • Business continuity arrangements 4 Principles The members will:‐ 4.1. At all times act in good faith towards each other. 4.2. Collaborate and co‐operate to deliver the agreed work programme. 4.3. Act in a timely manner. 4.4. Communicate openly about concerns, issues or opportunities relating to delivery of the agreed work programme. Page 1 of 12 20 November 2014 4.5. 4.6. 4.7. 4.8. Be accountable for the delivery of the agreed work programme and deployment of associated resources. Share information and experience to learn from each other. Adhere to statutory duties, laws and standards. Adopt a positive outlook and proactive manner. 4.9. Manage internal and external stakeholders effectively. 4.10 Seek to identify and manage any potential unintended consequences of collaborative decisions on individual members. 5 Responsibilities Services 5.1. Co‐ordinate the development an overarching strategic approach to collaborative commissioning across Lancashire and delivery within that approach of agreed collaborative programmes. 5.2. Ensure the public, partners and stakeholders are engaged in the development and delivery of the strategic approach. 5.3. Engage Health and Well Being Boards in the development of the strategic approach.. 5.4. Contribute to the development of member and partner strategies, for example Healthier Lancashire. 5.5. Identify and prioritise those service areas that will benefit from collaborative commissioning. 5.6. Identify the breadth of the collaborative arrangements, specifically which commissioning functions are included. 5.7. For each priority/project clearly identify and document the scope of the collaboration, decision making process and reporting arrangements. Specifically this should identify the mechanism for any collaborative decision making (paragraph 7.2 refers) and any associated decision making ‘gateways’. 5.8. Promote integrated commissioning and provision. 5.9. Promote innovation, research and evidence based practice. Contracts 5.10. Determine which providers and services to collaboratively contract and the underpinning arrangements. Programme Management 5.11. Ensure that robust programme management arrangements are in place for the delivery of the agreed work programme. 5.12. Ensure that component projects remain aligned to the Strategy and fit together properly, Page 2 of 12 20 November 2014 maximising opportunities for working across projects. 5.13. Ensure clinical and managerial resources are allocated from member organisations and commissioning support providers to successfully achieve project outcomes. Commissioning Support 5.14. Identify and secure the commissioning support required to underpin the collaborative commissioning arrangements. 6. Process for programme management 6.1 The general procedure for new programme consideration and overview of current programmes by the CCB is shown in Appendix A. This includes the Gateway reviews that CCB will be conducting on programmes. Steps between the Gateways may vary according to the nature of the programme or project. 6.2 In between the gateway reviews, CCB should seek simple assurance via the SRO that the programme is on track to deliver against milestones or be aware of the implications of any potential deviation. Should a risk or issue arise that could have significant strategic importance to CCB and / or its constituent members then CCB may call for a more detailed review paper. 6.3 All programmes will be underpinned by resource plans, detailing clearly how collaborative resource across CCGs, CSU, SCN, NHSE and others is anticipated will be applied in the delivery of programmes. Where application of resource to delivery of programmes varies significantly from plans, this should be escalated to CCB for review. Where PIDs for new programmes highlight additional resource requirements, CCB may consider the relative priority of the programme against others already underway. 6.4 The CCB should conduct an annual review of programmes to ensure that work is aligned to 2 year and 5 year plans, delivering on the highest priorities and focused on the areas of greatest complexity and maximum value. 7. Management of Programme Change Control 7.1 Change Control should be applied such that approval is sought from the lowest appropriate level within the programme hierarchy. Any substantive changes to previously approved programmes and/or programme documents should require re‐submission and approval of changes. 7.2 Papers submitted to boards / groups for approval of changes to agreed programmes should usually set out the reason for making the change and any known risks or impacts from the change as well as details of the change itself. Where the requested change impacts upon the resource plan, this should be highlighted in the paper to the CCB. 7.3 All transformation or development projects should have a means by which they report into either one of the programme boards or to CCB. This hierarchal structure maintains clear lines of reporting for projects to avoid ambiguity, which ensures that all transformation activity can be developed in a coherent, structured, integrated approach with consideration to inter‐dependencies and potential impacts across the whole system. Page 3 of 12 20 November 2014 8. Membership a) Chair Role Name Dr Amanda Doyle Title Clinical Chief Officer b) Vice Chair Peter Tinson Chief Operating Officer c) CCG Representative and NWAS/111 Group Chair d) CCG Representative and Medicines Optimisation Group Chair e) Collaborative Operational Delivery Group Chair (1) f) CSU Customer Forum Chair g) CCG Representative and Vascular Senior Responsible Officer h) CCG Representative and Collaborative Commissioning Support i) CCG Representative and Mental Health and Dementia Senior Responsible Officer j) CCG Representative and LD/CAMHS Senior Responsible Officer David Bonson Chief Operating Officer Organisation Blackpool CCG Fylde and Wyre CCG Blackpool CCG Dr Tony Naughton Clinical Chief Officer Fylde and Wyre CCG Carl Ashworth Senior Executive ‐ Transformation Midlands and Lancashire CSU Roger Parr Chief Finance Officer Andrew Bennett Chief Officer Blackburn with Darwen CCG Lancashire North CCG Peter Tinson Chief Operating Officer Fylde and Wyre CCG Sarah Camplin Debbie Nixon Chief Operating Officer Blackburn with Darwen CCG Roger Parr Dr Mike Ions Clinical Chief Officer East Lancashire CCG Page 4 of 12 Deputy Hilary Fordham k) CCG Representative and Stroke/TIA Senior Responsible Officer l) CCG Representative m) Chief Finance Officer Representative n) Primary Care Co‐ commissioner o) Specialised Commissioner p) Local Authority Commissioner q) Local Authority Commissioner r) Local Authority Commissioner Jan Ledward Chief Officer Mike Maguire Mark Youlton Chief Officer Chief Finance Officer Martin Clayton Alison Rylands Commissioning Director Mike Banks Val Raynor Paula Spence Deputy Medical Director (Clinical Strategy) Interim Director of Commissioning, Adult Services Public Health Head of Strategic & Procurement, Adult Social Care Greater Preston CCG and Chorley and South Ribble CCG West Lancashire CCG East Lancashire CCG 20 November 2014 Karen Sharrocks NHS England Lancashire Area Team NHS England Specialised Commissioning Team Lancashire County Council Terry Mears/Dawn Butterfield Blackpool Council Blackburn with Darwen Council Head of Contracting and Commissioning (1) ‘Close down’ collaborative work streams will report to Collaborative Operational Delivery Group. 8.1 Attendees A Strategic Clinical Network representative will be invited to attend all meetings and other partner or member representatives will be invited to attend as necessary. This includes CCG and CSU staff who are supporting the delivery of priorities/projects. Page 5 of 12 20 November 2014 9 Authority Accountability and Governance 9.1 The Collaborative Commissioning Board reports to the member organisations through their representatives. 9.2 The Board will consider the commissioning issue and identify the most appropriate mechanism to seek a collaborative decision, either:‐ o Individual members may participate in collective decisions in accordance with their delegated authority. o Delegated authority may be requested and received from members in relation to individual projects. o The Board may recommend to members a decision for ratification. 9.3 Each member retains accountability for the commissioning of care for which they are responsible and in accordance with their statutory duties and schemes of delegation. 9.4 A simple structure of accountability is set out in Appendix B. This establishes a simple hierarchy that links all projects back to delivery of the CCGs’ Strategic Plans. 9.5 Appendix C shows the governance architecture for the CCB and the groups reporting to it. 10 Chair The Collaborative Commissioning Board will be chaired by a Clinical Commissioning Group Clinical Accountable Officer or Clinical Chair. 11 Role of the Senior Responsible Officer (SRO) 11.1 The SRO for each agreed programme should be a regular board member of CCB and therefore by default a senior executive of one of the member organisations. 11.2 The SRO is not just a named lead of the particular programme, but should take an active leadership role to ensure the programme plans are appropriate and progressing to design. The SRO will be the programme representative at CCB. 11.3 The SRO should support and promote the programme to colleagues, key stakeholders, members of the public, politicians and the media. The SRO may be required to provide updates to sister organisations and public boards. 12 Frequency of Meetings Meetings will be held monthly. 13 Agenda and meetings 13.1 The agenda will be set by the Chair. 13.2 The agenda and all relevant papers will be circulated at least five working days prior to the meeting. Items that are late but urgent and important for circulation outside of the above can be done so with approval from the Chair. Page 6 of 12 20 November 2014 13.3 The CCB will operate a ‘Management by Exception’ approach seeking assurance from lower programme / project groups that satisfactory progress is being made and risks / issues identified and managed. Review of details, actions and progress of projects should be addressed through other more appropriate meetings. 13.4 The Senior Responsible Officer (SRO) will be responsible for reviewing and signing off highlight reports and other papers with the Service Redesign Team (SRT) lead(s) and agree with the Chair the time required to present each item. The agreed time slot will be strictly adhered to during the CCB meeting 13.5 Standard format highlight reports will be produced to ensure consistency of information passing to each board. 13.6 All papers should be clear around the recommendations being made and the decisions required from CCB and reflect the purpose and responsibilities for the SRO, CSU and CCB members as detailed in table in Appendix D. 13.7 The SRO will normally be responsible for presenting the paper to the meeting following discussion with SRT lead(s). 13.8 Individuals presenting papers should assume everyone has read the paper and give a short overview of the papers and describe the recommendations and decisions required from CCB. Individuals who are not core members of CCB should arrange to attend the meeting at the allotted 13.9 time on the agenda to present their paper and leave the meeting at the end of their item. 13.10 Any updates to member’s own organisation’s meetings should use the same papers as last issued to the CCB to ensure consistency between public board meetings. 13.11 Each CCB member is responsible for ensuring appropriate briefings are provided to their own organisations in regard to programmes and projects 14 Quorum The Collaborative Commissioning Board meeting is quorate when 5 of the 8 CCGs in Lancashire are represented by their named representative or deputy. 15 Reporting The minutes of meetings will be issued to all members within 10 working days of the meeting. 16 Review The Terms of Reference and Membership of the Collaborative Commissioning Board will be reviewed annually by the members. Page 7 of 12 20 November 2014 – Overall CCB Process Programme Proposed No further action Draft PS developed by CSU PS revised by CSU Draft PS Agreed by SRO Draft PS Presented to CCB PS Not Approved by CCB – Further work required Gateway 1 – PS Approval Programme Scope (PS) Should be 1 – 4 pages briefly covering: • • • • • • Vision / Outline of programme Key Outcomes Aim and Objectives Benefits to be realised Interface / Governance Timeline and key milestones • • • • • PS Not Approved by CCB Programme Scope Approved by CCB PID Developed by CSU Assumptions In‐scope / Out‐of‐scope Risks Roles and Responsibilities SRO / Exec Sponsor Gateway 2 – PID Approved Programme Initiation Document (PID) • Detailed programme plans by project • Key metrics and reporting • Stakeholders • Communications Plan • Methodologies • Diversity & Inclusion Checklist Specification / procurement development Gateway 4 – Service Procured • • • • • • • Detailed timelines Detailed resource plans Financial Plan Interdependencies Risk and Mitigation Plans Options Appraisal Potential Procurement Service to be reprocured Service Mobilisation Monthly Programme Assurance Gateway 3 – Approach to securing service change agreed by CCB Review Implementation of Service Page 8 of 12 Option appraisal and case for change developed Gateway 5 Closure of Programme 20 November 2014 – Strategic Model Accountability and Quality Assurance Framework CCG / LA Public Boards Collaborative Commissioning Board Programme Boards & Operational Delivery Group CSU Internal Review Process Project Groups (as appropriate) Strategic Plans and Controls Overview Public Accountability Overall strategic plans & Clinical Accountability Programme Plans, Progress and Corrective Actions Individual project plans, actions, details and tactical changes Page 9 of 12 Change Control Strategic Direction Change Control Strategic Direction Change Control Strategic Direction 20 November 2014 Page 10 of 12 20 November 2014 Appendix D – responsibilities re management of papers Type of Paper/Report Purpose SRO Responsibility CSU Responsibility Decision For discussion and a decision by all CCGs Debate To discuss and • To introduce • To identify debate a subject subject and topics for e.g. to see if SME if in discussion of there is local attendance. local or national appetite for a relevance work stream or • To facilitate to raise • To provide discussion awareness of and gain sufficient particular or consensus information for local or national issues etc. on next background of steps subject matter to aid • To align discussions. workstream with agreed • To invite SME next steps to attend CAG where required CCG Responsibility • Present paper • To ensure there • CCG representative and facilitate is sufficient discussion to information in had sufficient discussion allow required the paper and decisions to suitable with local lead for subject be made. questions around matter to be able to make questions. a decision on • To ensure that behalf of CCG papers are out • To raise any in time to issues with enable local SRO or CSU discussions to lead for the take place programme • To ensure prior to the sufficient time meeting on agenda for brief discussion and decision Page 11 of 12 • To ensure • To read subject matter provided • To identify if there are local colleagues who need to also attend debate 20 November 2014 sufficient time on the agenda for debate • Provide Teleconference arrangements to encourage more participation from CCGs in debate Information Only Operational To provide brief (Highlight update of progress report Report) progress since last HL report to CAG Parking Lot To put work • To lead the • To manage (list which we streams on hold, discussion as this within add to and due to no to the next agreed criteria remove from) appetite, steps with for (don’t want it awaiting the to be a national/local programme dumping decision’s ground for the • The ensure “too hards”). regular review of ‘Parked’ • To review programmes/ each month projects with a brief comment on list and update at CAG Page 12 of 12 To note progress and share with local CCG • To support discussion at CAG and recommendati ons to “close” programmes/ projects. GOVERNING BODY MEETING Date of Meeting 14th January 2015 Title of Report Agenda Item No. Planning Guidance 2015/16 – Year 2 Update Governing Body Responsible Officer Mr Roger Parr, Chief Finance Officer Summary/Purpose of Report Governing Body Action 19 Lead Clinician Lead Manager Mrs Claire Moir, Governance, Performance and Risk Manager The purpose of this report is to provide the Clinical Commissioning Group’s (CCG) Governing Body with an overview of the requirements outlined within the planning guidance (2015/16) which was published by NHS England on 23rd December 2014. The Governing Body is requested to: • Note the contents of the report Please indicate the Committee(s)/Group(s) where the paper has been discussed/developed Operations and Delivery Group Please note the following section must be completed in full Patient and Public Yes Undertaken as part of the development of the CCG Engagement 5 Year Strategic Plan Completed Equality Analysis Yes Equality Analysis Assessment undertaken on the Completed CCG 5 Year Strategic Plan Financial Finance and Activity templates will be populated as part of Implication(s) the planning process Risk(s) Identified Any risks identified will be managed through the planning and delivery process CCG Strategic Objectives supported by this paper 1. We will continuously improve the health and well-being of the population of Y 2. 3. 4. 5. Blackburn with Darwen. We will build successful partnerships which promote collaborative working and integrated service delivery. We will effectively engage patients and the public in decision making. We will co-commission and deliver continuous improvement in Primary Care Services and tackle inequalities. We will commission safe and effective services for the population of Blackburn with Darwen with integration at the heart of commissioning. Y Y Y Y CCG High Impact Changes supported by this paper 1. 2. 3. 4. 5. 6. 7. 8. 9. Delivering high quality Primary Care at scale and improving access. Self-Care and Early Intervention. Enhanced and Integrated Primary Care and Better Care Fund. Access to Re-ablement and Intermediate Care. Improved hospital discharge and reduced length of stay. Community based ambulatory care for specific conditions. Access to high quality Urgent and Emergency Care. Scheduled Care. Quality. Page 1 of 4 Y Y Y Y Y Y Y Y Y Planning Guidance – 2015/16 Year 2 Update 1. Introduction 1.1 The purpose of this report is to provide the Clinical Commissioning Group’s (CCG) Governing Body with an overview of the requirements outlined within the planning guidance (2015/16) which was published on 23rd December 2014. 2. Planning Guidance – Key Headlines 2.1 All existing objectives from the 2014/15 mandate have been carried over with 2 important updates: • • To join up health and social services through the Better Care Fund To introduce access and waiting time standards in mental health by March 2016 2.2 The 2015/16 mandate remains structured around the 5 domains of the NHS Outcomes Framework. Whilst there is no requirement to upload a narrative operational plan as part of the national submission process, there is an expectation that CCGs will produce narrative annual plan to demonstrate progress with the outcome framework indicators and trajectories to be achieved during the 2015/16 financial year. 2.3 Additional supplementary information has also been provided which outlines further information for planning and business rules for 2015/16. The guidance also sets out the fundamental requirements for all commissioning plans under the following headings: • • • • • Outcomes o Delivery across 5 domains and seven outcome measures o Improving health o Reducing health inequalities o Parity of esteem Access o Convenient access for everyone o Meeting NHS Constitution standards Quality o Responses to Francis, Berwick and Winterbourne View o Patient safety o Patient experience o Compassion in practice o Staff satisfaction o Seven Day Services o Safeguarding Innovation o Research and Innovation Delivering Value o Financial resilience; delivering value for money for taxpayers and patients and procurement Page 2 of 4 3. Operational and Planning Measures 2015/16 3.1 Detailed operational plan measures which formed part of the 2 year operational plans submitted in 2014/16 will need to be reviewed and refreshed. Key changes for 2015/16 are highlighted in the guidance and include a requirement for inpatient activity plans to be based on spells as used in the Secondary Uses Service (SUS) data. Additionally, as the CCG intends to apply to NHS England for delegated commissioning responsibilities, additional primary care metrics will also need to be included as part of the year 2 refresh process. 3.2 Activity and financial planning data templates have been provided for completion by commissioners in line with national timescales (see below). This year more emphasis has been placed on finance associated with activity which will be considered and aligned to the contracting process for 2015/16. 4. Planning Requirement Timescales 4.1 Attached at Appendix 1 is an outline of the actions required against the national timescales. 5. Next Steps 5.1 The CCG’s Operational Delivery Group will undertake and coordinate the work required to ensure the operational and planning measures are reviewed and refreshed, and that the 2015/16 narrative annual plan is developed in accordance with the guidance. 5.2 The Governing Body will receive progress reports at both the February and March meetings prior to final submission of the planning templates to NHS England. 6. Recommendations 6.1 The Governing Body is asked to: • Note the contents of the report Mr Roger Parr Chief Finance Officer 7 January 2015 Page 3 of 4 Appendix 1 Planning Requirements Timescales Date Action 13 Jan 15 1st cut of activity trajectories submitted via UNIFY From 29 Jan 15 onwards Weekly contract tracker to be submitted (Thursdays) 13 Feb 14 Checkpoint 1 – feedback on progress with planning measures and trajectories 20 Feb 2015 National contract stocktake 27 Feb 2015 Submission of full draft plans 27 Feb ‐ 30 Mar 15 Assurance of draft plan 6 Mar 15 Checkpoint 2 – further feedback on plans 11 Mar 15 12‐23 Mar 15 25 Mar 15 Contracts signed post mediation Contract arbitration Arbitration outcomes notified to commissioners 31 Mar 15 Plans approved by CCG Governing Body 10 Apr 15 Submission of full final plans 10 Apr 15 onwards Assurance and reconciliation of operational plans Page 4 of 4 GOVERNING BODY MEETING Date of Meeting Title of Report Governing Body Responsible Officer Summary/Purpose of Report 14TH JANUARY 2015 Agenda 20 Item No. GOVERNING BODY SUB COMMITTEES AND GROUPS’ SUMMARY Lead Clinician Lead Manager This document summarises each Committee Meeting for the Governing Body (GB), identifying key decisions, recommendations and items of particular interest. Full copies of the minutes are available from the Corporate Support Officer, if required. The Governing Body is requested to note the content of the report. MR IAIN FLETCHER, HEAD OF CORPORATE BUSINESS Governing Body Action Please indicate the Committee(s)/Group(s) where the paper has been discussed/developed Commissioning Business Group Audit Committee Quality, Performance and Effectiveness Committee Lancashire Clinical Commissioning Group Chairs’ Network Blackburn with Darwen Health and Well-being Board N/A Result Patient and Public Engagement Completed Equality Analysis N/A Result Completed None Financial Implication(s) None Risk(s) Identified CCG Strategic Objectives supported by this paper 1. 2. 3. 4. 5. We will continuously improve the health and well-being of the population of Blackburn with Darwen. We will build successful partnerships which promote collaborative working and integrated service delivery. We will effectively engage patients and the public in decision making. We will co-commission and deliver continuous improvement in Primary Care Services and tackle inequalities. We will commission safe and effective services for the population of Blackburn with Darwen with integration at the heart of commissioning. Y Y Y Y Y CCG High Impact Changes supported by this paper 1. 2. 3. 4. 5. 6. 7. 8. 9. Delivering high quality Primary Care at scale and improving access. Self-Care and Early Intervention. Enhanced and Integrated Primary Care and Better Care Fund. Access to Re-ablement and Intermediate Care. Improved hospital discharge and reduced length of stay. Community based ambulatory care for specific conditions. Access to high quality Urgent and Emergency Care. Scheduled Care. Quality. Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 1 of 29 CLINICAL COMMISSIONING GROUP (CCG) GOVERNING BODY MEETING 14TH JANUARY 2015 GOVERNING BODY SUB-COMMITTEES AND GROUPS’ SUMMARY 1) Introduction This document summarises each Committee Meeting for the Governing Body (GB), identifying key decisions, recommendations and items of particular interest. Full copies of the minutes are available from the Corporate Support Officer, if required. 2) Commissioning Business Group (CBG) Chair – Dr Muzaffar Pervez, General Practitioner (GP) Executive The members present declared their conflicts of interest to the appropriate agenda items. 2.1 Minutes of the Meeting held on 12th November 2014 a) Proposed Pennine Lancashire Cancer Local Improvement Scheme 2015/16 A power point presentation was given by Dr Neil Smith, GP Lead for Cancer and CBG were asked to consider the future funding of the Local Improvement Scheme (LIS). Proposed LIS is to maintain a practice core team and continue training. Recommend that Blackburn with Darwen (BwD) CCG support the scheme and confirm to NHS England. b) Drug and Alcohol Misuse Prevention and Recovery Services Tender Prime Provider Model. The paper set out what has already been achieved and what is being proposed for the future of commissioning these services. A number of stakeholder workshops have been held, with the main outcomes being improving recovery with a prime provider model. CBG asked to note the process being undertaken by Public Health. c) Primary Care Resilience GP access over the holiday period, was discussed within the context of Annual Resilience funding. The various different initiatives were discussed: • In house additional appointment • Longer weekly opening hours • Weekend working Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 2 of 29 There was recognition that a decision needed to be made swiftly in order for practices to mobilise. 2.2 Minutes of the Meeting held on 10th December 2014 a) Calculating the Quality Premium 2013-14 The purpose of the paper was to provide a final position relating to the 2013/14 Quality Premium. b) Scheduled Care Demand Management – Community Care Development The purpose of the paper was to outline the proposed developments across community services within a primary/community setting as part of the wider scheduled care demand management initiative. c) Faecal Calprotectin Testing CBG were asked: • • • To support the development of a Faecal Calprotectin pathway in partnership with East Lancashire Hospitals NHS Trust (ELHT). To support the implementation of Faecal Calprotectin testing within secondary care To consider, and approve or otherwise, the proposal to develop a Faecal Calprotectin primary care screening service for patients with suspected inflammatory bowel disease. The clear benefits associated to the use of Faecal Calprotectin testing, including improved patient experience, and considerable cost benefits were discussed. The implementation of the test within secondary care can be established within short timeframes. d) Primary Care Co-Commissioning – Primary Care Development and Assurance Group Terms of Reference (ToR) A general update was given in terms of the group and ToRs already established. At the last GB and Senate it was agreed that BwD would go with full delegation rights, and letters have been issued to all Practices and the Health/Social Community. It was agreed that this had to be a separate Committee to GB and CBG, although it may follow on from one of these meetings to allow for quoracy. Noted and accepted the paper. Action: Needs to come to CBG in February for GB in March – with agreed positions in place. e) Scheduled Care Highlight Report No action is required, the paper was noted f) Prescribing Update – Quarter 2 Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 3 of 29 The increased drug costs are putting pressure on BwD CCG, with no direct control of the expenditure of the prescribing. The Medicines Management are working to manage these cost pressures. The paper was noted and comments passed to Medicines Management, no action required. g) Any Other Business Primary Care Access over Holiday Period 26 practices offering additional in hour appointments. Working at promoting these centrally through Communications. Mrs Lisa Kiernan, Head of Primary Care and Integrated Community Services, to link with East Lancashire Medical Services and 111 re the practice data and to include BwD North practices for appointments they don’t use. 3) Quality, Performance and Effectiveness Committee (QPEC) Chair – Dr Nigel Horsfield, Lay Member – Secondary Care Doctor (Retired) 3.1 Minutes of the meeting held on 8th October 2014 a) Performance Report & Appendix 1 & 2 Mr David Rintoul, Performance and Quality Specialist and Mr Michael Connell, Quality and Performance Support Officer, jointly presented the Month 4 Quality and Exception Report produced by the Midlands and Lancashire Commissioning Support Unit (CSU). b) Lancashire Care NHS Foundation Trust Improving Access to Psychological Therapies: Continued improvement demonstrated across Lancashire with the notional 1.25% monthly target being exceeded @ 1.29% The trust is projecting that all CCG areas will be compliant with the national target by February 2015. The trust is actively engaging with disparate and hard to reach groups to meet the prevalence target including employers premises (BAE Systems) veterans, perinatal women, older adults, young men and Asian heritage women. Memory Assessment Service (MAS): Errors have been identified in the trusts recent data submissions which have meant that their levels of compliance with the 3 day triage target have been overstated. These have now been resolved. Consultation is underway with other commissioners regarding the removal of this target as it is felt to be ineffective and poor utilisation of resources now that waiting times have reduced significantly. 60.5% of BwD patients met the 4 week treatment target in July, below the 70% target, but a significant increase on the June figure of 33.3%. The trust has highlighted incomplete referrals as being a major contributory problem to delays in treatment, particularly in Chorley South Ribble/GP areas. Care Programme Approach (CPA): CPA 7 day follow up continues to be an issue with Blackpool in particular. All other areas are meeting the 95% target on a year to date basis. The trust continues to provide detailed breach reports on each individual breach but the % effect of each breach is significant because of the low numbers involved. Falls Assessment: It was reported that in a previous edition of the report concerns were raised around falls at Lancashire Foundation NHS Trust (LCFT). It has been agreed in future to include a specific update on adult mental health wards and are working with the trust to improve reporting in this area. Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 4 of 29 d) ELHT Cancer 62 day wait: The target for 85% of patients to receive first definitive treatment for cancer within 62 days is not being met on a year to date basis. BwD patients stands at 81.3%. To meet the trajectory BwD CCG need to have less than 4.5 breaches per month from now until the end of 2014/15. As this target may be difficult to reach initiatives were given to the committee to consider. Stroke: Currently not meeting 90% for last quarter of patients admitted to the stoke unit within 4 hours. Improvement measures have been maintained at 50.46% for 2013/2014, 61.4% in July and figure to date for September show a huge improvement of 77.76%. Friends & Family Test: The response rate to date for ELHT is 8.3% failing both the Commissioning for Quality and Innovation Payment Framework Target (CQUIN) of 15% and the Trust Development Authority target of 20%. The trust is due to report back some analysis around the friends and family test as part of its Q2 Commissioning for Quality and Innovation (CQUIN) reconciliation process next month. Accident and Emergency (A&E) 4 Hour: To note the Trust did meet the 95% target in July but has failed in both August and September at 93.49% and 94.55%. The trust is looking at implementing a new e) Other Providers North West Ambulance Service: Significant deterioration in RED 1 performance in BwD over the last few months. North West Ambulance Service has been missing the 75% target overall for several months but meeting the target in BwD. f) BwD CCG Balanced Scorecard July 2014 Clostridium Difficile: Current position nine over trajectory. Post Infections reviews have been completed on all nine cases of which were deemed to be unavoidable. Seven were attributed to ELHT and the remaining two are community acquired. ELHT to carry out a route cause analysis. Francis/Keogh/Berwick Update: Mrs Kim Smith, Head of Quality, confirmed that actions from main providers are to be taken to the Lancashire Quality and Performance meeting and to be brought back to the committee monthly. g) Business Items BwD Public Health Research and Development Update: Ms Ruth Young, Public Health Consultant, outlined the report which is to highlight progress on identified shared priorities and to consider opportunities to work with the National Institute for Health Research Collaboration (CLAHRC) Safeguarding – BwD Engage – Child Sexual Exploitation Update: Ms Rebecca McGeowan, Lead Clinician, provided the committee with a summary of the national updates and recommendations regarding child sexual exploitation and an overview of the existing developments locally. Risk Management Report Quarter 2 Update: Mrs Claire Moir, Governance, Performance and Risk Manager, updated the committee on the current risks held on the full corporate risk register and asked the committee to note the contents of the report and approve the closure of Risk 2014/03 - Risk of service disruption due to notice served by East Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 5 of 29 Lancashire CCG to ELHT for Dermatology, Ophthalmology and Musculoskeletal service. Risk 2014/05: Failure to achieve all levels of Quality, Innovation, Productivity and Prevention (QIPP) savings 2014/15. Risk ID 2014/06: There is a risk that the CCG will be unable to accurately forecast the year-end financial outturn due to individual patient activity services being inaccurately reported within the Broadcare Database system. Assurance has been given that the information in the database is now correct, spot checks will continue to be carried out and the risk managed operationally. Conclusion: Risks approved for closure In addition, Mrs Moir asked for the following new risks to be included on to the Corporate Risk Register. 2014/08 - There is a risk that regional requirements to attain RED 1 and RED 2 targets for emergency services will not be met. 2014/09: There is a risk that scheduled care service re-design across Pennine Lancashire may not be aligned between East Lancashire and BwD CCG leading to differences in configuration and inequity of provision. Conclusion: Risks approved for inclusion. Cancer Update: Dr Smith provided committee members with a presentation on the important cancer care targets from April 2014 – March 2014 and also the proposed governance arrangements for the Pennine Lancashire Cancer Programme Board. Dr Smith further outlined the financial penalty that each CCG will lose if they do not reach target. Lengthy discussion with regards to the various breach reasons across the trust which related to 66% of all breaches plus a further breakdown of all reasons given on Open Exeter by patient choice. Lengthy discussion on the reasons why BwD consistently fail to reach target compared to East Lancashire raised concern amongst committee members. Mrs Lynn Scott, Service Redesign Manager, confirmed that East Lancashire CCG are to advertise for a cancer tracker to pull out urgent GP referrals to help manage a patients journey through the system. 3.2 Minutes of the meeting held on 29th October 2014 a) BwD 62 Day Cancer Recovery Plan: Mrs Scott and Ms Juliette Mottram, Cancer Services Manager, were asked to attend the meeting and provide a further understanding of the various issues across the cancer pathways and whether it would it be possible to get a list of all patients who are at 40 days and then pull those patients to see how far they are along the pathway and to see what could be done to prevent them from breaching. Ms Mottram informed the Committee that the service are already doing this, and outlined the various multidisciplinary team/tracker/hot clinics/ meetings that are held weekly to try and pull out the various patients that may breach and pull them through the system. Ms Mottram said that an analysis of the breaches for BwD has been carried out to which it was noted that patient choice was a one of the factors for the breaches as there appears to be a reluctance from patients to attend the unit at the Burnley site, and that some patients who need a bowel screening scope are going to Preston. Conclusion: The committee thanked Mrs Scott and Ms Mottram for attending but commented that they felt less assured than previous and that there was now an acceptance amongst the committee that BwD would fail to reach target and therefore the recovery plan needs to be explicit regarding actions to be taken with clear timescales Action: Escalation of BwD 62 day cancer breaches to be raised with Dr Chris Clayton, Clinical Chief Officer, and Governing Body members that BwD will not reach target. Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 6 of 29 b) Performance Report and Appendix 1 & 2 Mr Connell presented the Month 5 Quality and Exception Report produced by the Midlands and Lancashire CSU. c) LCFT Improving Access to Psychological Therapies: Prevalence rates have fallen in August to below the 1.25% notional target at both Trust level and for BwD patients. The Trust are continuing to look to improve rates via promoting the self-referral pathway aimed at target groups. Recovery rates remain below 50% target for al CCG’s at 36.72% Trust and 34.48% for BwD patients. Memory Assessment Service (MAS): The target of 70% of patients triaged within 3 days by the MAS was met across the trust in August with the exception of Blackpool. Monitor: LCFT Continuity of Service Ratings. The risk that the Trust will fail to carry on as a going concern has been downgraded from 4 to 3. As a result of the Trusts financial position at month 1, where the Trust have reported a deficit due mainly to out of area treatments and cost improvement failures. Since month 1 the Trusts financial position has improved and they expect to move back up to 4 at the end of Quarter 2. National Reporting and Learning Systems: To note that both trusts show lower degrees of harm, however it was noted that LCFT are showing a significantly higher number of incidents than other mental health organisations. d) ELHT National Cancer Patient Experience Programme: Results from the survey show a downward trend with only the question around patients bringing a friend with them to appointments shows an improvement. 18 weeks referral to treatment: 3 specialties failing 18 weeks Refer to Treatment (RTT) at Ear Nose and Throat, Urology and Oral Surgery. It was noted that more narrative is needed from the Trust. A&E 4 Hour: The Trust failed the 95% target in August at 93.49% under performance attributed to bed capacity and patient flow. Stroke 4 hour target: August performance of 68.67% against the stroke 4 hour target, which is below the 90% local quality requirement but is still an improvement from previous years. Friends & Family: A&E response rates remain low and are below CQUIN target of 15% for the 3rd consecutive month at 12.6%. e) North West Ambulance Service Red 1 and Red 2 Emergency Calls – Performance has improved against both Red 1 & Red 2 response time targets with the CCG position of 82.35% and 77.72% against a target of 75%. To note the CCG’s quality premium is linked across the whole of the Trust on a year to date position. Mrs Smith confirmed that a meeting with all providers looking at the number of increased failings is to be addressed shortly. f) NHS Constitution: The CCG is currently rated Red for 6 NHS Constitution measures in August 2014: 4 Hour A&E waiting times; 31 day cancer subsequent treatment waits; 62 day Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 7 of 29 cancer 1st definitive treatment waits; 62 day NHS Cancer Screening Service waits; Ambulance Red 1 response times; and Ambulance Red 2 response times. g) Business Items Safeguarding Review Action Plan: Mrs Sue Clarke, Head of Safeguarding, outlined the purpose of the review which was to understand the governance arrangements and the capacity within the CCG to deliver statutory functions and inform future commissioning arrangements. Strategic Clinical Network Care Education Standards for Care and Support for the dying person: The Committee noted the contents of the report and agreed the process and the suggested monitoring arrangements. Risk - Risk Management Report – Quarter 2: Mrs Moir asked the Committee to note the contents of the report and said that at present there are currently no new risks for inclusion on the corporate risk register and also that there are no risks recommended for closure. ACTION: Following discussions with committee members around the 62 day cancer recovery plan it was agreed to increase Risk 2013/08 to 15 – Increase Risk CO4.2 to 16 as committee members were in agreement that there is added risk around the financial element of the CCG’s co-commissioning bid of delegated responsibility and to reduce 2014/02 to 9 following Mr Keith Dibble’s confirmation that LCFT’s protocol has now been signed off and in place. To be reviewed in 3 months. 3.3 Minutes of the meeting held on 26th November 2014 a) Mr Stuart Sheridan, Learning Disabilities and Complex Needs Manager, provided the Committee with an overview of the national response following the Winterbourne Hospital 2011 abuse allegations and outlined the actions and locally agreed joint plan aims that are in place, plus the next steps to reduce admissions and out of borough placements of children and young people across BwD. To Note: Mr Sheridan asked the Committee to note that there are currently 20 people in different types of hospitals at a cost of approximately £1.5 million. b) Performance Report and Appendix 1 and 2 Mr Rintoul and Mr Connell Performance Support Officer presented the Month 6 Quality and Exception Report produced by the Midlands and Lancashire CSU. c) LCFT Improving Access to Psychological Therapies (IAPT): The notional 1.25% target for prevalence was not met in September at CCG level or provider level, however there was some slight improvement in August. Referral rates in all areas are below that required to meet the 15% target to which the trust are implementing a wide range of strategies to increase referrals in particular self-referrals. Mr Rintoul asked the Committee to note that the planned relaunch of the IAPT service under the ‘Minds Matter’ is now underway. Memory Assessment Service (MAS): The 70% target for patients to be seen within 4 weeks was not met in any CCG area in September with 57.5% being seen in BwD and 42.19% on a trust wide basis. The average wait in BwD was 7.4 weeks below the trust average of 11 weeks. Poor quality referrals continue to be an issue. Mrs Smith commented that the referral criteria for this is to be challenged next year. Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 8 of 29 Care Programme Approach: Blackpool continues to be reported as not achieving whilst other areas are. Reporting errors within LCFT have been identified and raised with the Trust. An internal investigation is currently underway and it is likely that there will be some revision of previously submitted information. CQUIN: Mr Rintoul confirmed that of the 8 CQUIN Schemes 5 have met target, 1 has not met and the remaining 2 are not due to report this quarter. The friends and family test scheme is not meeting the target which is due to a combination of national delays and poor implementation within the trust. d) ELHT Cancer: The trust met the 62 day cancer target in September at 90.33% but is failing the year to date position at 82.78%. Pennine Lancs 62 Day Cancer Waiting Times Business Plan: The Committee noted the contents of the business assurance plan and commented that they are all still not assured that the trust will meet target. A&E 4 Hour: It was noted that East Lancashire Hospitals trust have failed the 95% target in September at 94.55%. A&E targets are failing nationally with a national figure of 92.9%. Underperformance was attributed to bed capacity and patient flow pressures. Improvement measures at the trust include the development of triggers and responses for earlier escalation and the development of a live data feed of performance to support escalation and the introduction of earlier discharges in the day. Stroke 4 hour: Performance against the stroke 4 hour admission target has declined in correlation with A&E performance. 60% of patients were admitted to the acute stroke unit within 4 hours in September. Medical bed capacity was attributed to one of the causes. North West Ambulance Service: The Red 1 and Red 2 response time targets have been met at CCG level with performance at 81.63% and 82.02% against a target of 75% in September. However as previously discussed the CCG’s quality premium is linked to performance across the whole of the trust on a year to date position which is still failing due to performance in other areas. A&E Benchmarking: Analysis carried out around A&E attendances across Lancashire shows that BwD has a significantly low level of A&E attendance which stands at 6% below expected levels. It was noted that patients in the East locality have the higher rate of attendance to the A&E department. Outpatient Benchmarking: Mr Rintoul gave an overview of the two specialties currently experiencing significant overtrades at the trust which are pain management and trauma and orthopaedics. e) Safety Insulin Incident Update Response Diabetologists: Dr Malcolm Ridgway, Clinical Director for Quality and Effectiveness, provided the Committee with a brief overview of the insulin incident and the investigations that was carried out. CONCLUSION: It was noted that as no harm was caused to the patient this is not classed as a never event. Safeguarding Quarterly Report: Mrs Clarke provided the Committee with the first Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 9 of 29 quarterly update report which in the future is to be presented dashboard style. Conclusion: The Committee noted the contents and the identified risks. Pan Lancashire Child Death Overview Panel Annual Report 2013 -2014: Dr Gifford Kerr, Public Health Consultant, provided a summary of the sixth annual report since the Child Deaths Overview Panel became statutory in April 2008. Dr Kerr asked the Committee to note that the number of notifications received in each reporting year since becoming statutory in 2008 shows a decline in child deaths. It was noted that chromosomal, genetic and congenital anomalies are the largest category of death for BwD. f) Risk Risk Management Report: Mrs Moir asked the Committee to note the contents of the report and approve the inclusion of one new risk 2014/10 Risk to inappropriate arrangements made under the Mental Health Capacity Act Deprivation of Liberty Standards to the register and to approve the closure of Risk ID 2014/09 Risk that the service re-design models in scheduled care are not aligned resulting in inequity of service across Pennine Lancashire. CONCLUSION: Chairs Actions: Recommendations approved. 4) Audit Committee Chair – Mr Paul Hinnigan, Lay Member – Governance Minutes of the Meeting held on 22nd October 2014 a) Apologies for Absence and Confirmation of Quoracy Apologies were received. The meeting was confirmed as quorate. b) Minutes of the Meeting held on 4th June 2014 The minutes of the meeting of 4th June 2014 were reviewed and approved as an accurate record. RESOLVED: That the Minutes of the Meeting held on 4th June 2014 were approved as an accurate record. c) Matters Arising Minute 14.006.4 – External Audit – Key Issues for CCGs – National Update Mr Roger Parr, Chief Finance Officer, provided feedback on the issue relating to pharmaceutical companies’ discounts, which was one of the ‘top ten issues’ identified in the national update. Mr Parr confirmed that there were no issues locally. d) Minute 14.039.1 Audit of Annual Accounts and Financial Statements and Review of External Audit Opinion – Value for Money Conclusion The Chair reported that the action related to a number of Information Technology (IT) issues had been discussed during a Governing Body (GB) meeting. e) Risk Management Report Mrs Claire Moir, Governance, Performance and Risk Manager, presented the Risk Management Report, which provided members with an update on the management of risks held on the Corporate Risk Register (CRR) for the period April – September 2014. Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 10 of 29 At the GB meeting in August, 10 risks were identified and assigned to a Senior Officer in the CCG. The CRR is presented to the QPEC every month to approve or remove risks; discussed at the Executive Team and Operations Group and also reviewed by the Clinical Chief Officer on a monthly basis. The Governing Body Assurance Framework (GBAF) is reviewed by the GB on a quarterly basis and the dates for review were provided in the report. It was noted that some risks may continue to be monitored by the QPEC on a monthly basis, even if the target was being achieved. Members of the Audit Committee (AC) agreed that they were satisfied with the adequacy of the systems of internal control within the CCG and that the processes in place appeared to be robust. RESOLVED: That the Audit Committee noted the content of the report. f) External Audit Progress Report Mrs Karen Murray, Director, Assurance, Grant Thornton UK LLP, presented the first progress report for this year, which provided the AC with a report on progress of the delivery of External Audit’s responsibilities for 2014/15. Mrs Murray added that audit work has not yet commenced but there would be an interim visit to the CCG within the next few months. It was noted that, once the Department of Health (DH) had notified CCGs of the 2014/15 pre-audit and post-audit final accounts deadlines, AC meetings would need to be coordinated with the deadlines. Mrs Murray drew members’ attention to the emerging issues and developments section of the report which highlighted matters the CCG needed to be made aware of and the section which reflected on the process of the preparation and audit of the CCG financial statements for 2013/14. Mrs Murray invited comments from the CCG on how the process could be improved for 2014/15. Annual Audit Letter Mr Chris Whittingham, Manager, Assurance, Grant Thornton UK LLP, presented the Annual Audit Letter for 2013/14, which was the final element of the audit process and brought it to a close. Mr Whittingham highlighted key elements of the letter: • • • Auditing the 2013/14 accounts Final statements opinion Value for Money conclusion Mr Whittingham reminded members that the Audit Findings report had been presented to the June meeting of the AC. He confirmed that there had been no issues for the group auditor to consider and that all deadlines had been met. Mr Whittingham stated that, once guidance was available from the DH, he would meet with Mr Parr to discuss planning for 2014/15. He confirmed that the audit fee for 2014/15 would be in line with expectations. Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 11 of 29 RESOLVED: That the Audit Committee noted the content of the reports. g) Internal Audit Progress Report Mrs Lisa Warner, Senior Internal Audit Manager, Mersey Internal Audit Agency (MIAA), presented the Progress Report which provided an update to the AC in respect of the assurances, key issues and progress against the Internal Audit Plan 2014/15. Mrs Warner drew members’ attention to key messages; one of which related to a report regarding the Quality of Commissioned Services and the subsequent actions required by the CCG. The report concluded that there were good systems and processes in place with just three recommendations. Mrs Warner reported that all the recommendations for 2013/14 had been actioned. Mrs Warner outlined work in progress, which would be reported to the AC following completion. She assured the AC that the plan would be delivered by the end of the financial year. Mr Parr reported that he had met with Mrs Warner to discuss the plan and ensure that delivery remained on track. He had also discussed the Quality of Commissioned Services Report with Mrs Kim Smith, Head of Quality and the three recommendations within the report would be addressed via the QPEC. Charter The Internal Audit Charter is mandated through the Public Sector Internal Audit Standards (2013) and is a formal document that defines the internal audit activity’s purpose, authority and responsibility. Mrs Warner requested that the AC consider and approval the Internal Audit Charter. Audit Committee Handbook Briefing The briefing provided a summary of the key changes to the revised AC Handbook that was issued in June 2014. It was suggested that the AC may wish to review its Terms of Reference in light of the changes. MIAA Briefing – Sustainability and Human Factors The two briefings produced by the MIAA were circulated for information and in order for the CCG to consider its own arrangements. Clinical Commissioning Group Assurance Framework Benchmarking Report Mrs Warner provided an overview of the report which set out the results of a recent benchmarking exercise undertaken by MIAA on CCGs GBAFs. It was noted that Blackburn with Darwen CCG had been included in the exercise. The report provided an opportunity for CCGs to compare key elements of their frameworks to other CCGs. RESOLVED: That the Audit Committee: • noted the content of the reports Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 12 of 29 • approved the content of the Internal Audit Charter. h) Anti-Fraud Progress Report Mrs Clare Ward, Local Counter Fraud Specialist, presented the progress report in the absence of Mr Roger Causer. Mrs Ward informed the AC that Mr Chris Morris, Senior Counter Fraud Service Manager, was leaving the MIAA and Mr Causer was the Interim Senior Counter Fraud Service Manager whilst a replacement was being recruited. The report set out the work undertaken during the period of April – September 2014 and highlighted activities and outcomes to be brought to the attention of the AC. Section 2 of the report indicated the type of work agreed in the plan for the financial year with Mr Parr and progress made against each area of work. Sections 3 and 4 indicated any detailed findings and investigations summaries respectively. Following an enquiry from the Chair, Mrs Ward assured the AC that the full plan would be delivered by the end of the financial year. RESOLVED: That the Audit Committee noted the content of the report. i) Losses and Special Payments: Mr Parr presented the Losses and Special Payments report. There were no losses or special payments made during the period 1st April – 30th September 2014. RESOLVED: That the Audit Committee noted the losses and special payments made during the period 1st April – 30th September 2014. j) Waivers and Standing Orders Mr Parr presented the Waivers and Standing Orders report. There were two single tender waivers for the period 1st April – 30th September 2014. RESOLVED: That the Audit Committee noted the single tender waivers recorded for the period 1st April – 30th September 2014. k) Gifts and Hospitality/Register of Interests Mr Parr presented the Registers Update. Mr Parr reported that the CCG was in the process of completing its Staff Register of Interests (not including members of the GB who were included in a separate register published on the CCG’s website) but the quality of information was not of a standard to meet the requirements of the national template distributed by NHS England. There were plans to complete the register on a face to face basis and then it would be brought back to a future meeting of the AC. Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 13 of 29 There were several entries to the Gifts and Hospitality Register since the last meeting of the AC. The entries related to vouchers received by the Chairman for work to complete online surveys and would be used in staff incentive schemes. RESOLVED: That the Audit Committee noted the current position related to Gifts and Hospitality/Register of Interests. l) Out of Pocket Expenses Update Mr Parr presented an update on the current position related to Out of Pocket expenses. This was a legacy issue from the former Care Trust Plus. RESOLVED: That the Audit Committee noted the content of the update. m) Consultation of Consultation of Regulations for NHS Bodies’ Auditor Panels The Chair presented the draft regulations developed by the DH to implement new constitutional requirements for ACs (acting as auditor panels) of NHS Trusts and CCGs for information and to bring to members’ attention that the consultation had taken place and the outcome was awaited. RESOLVED: That the Audit Committee noted the content of the proposed regulations. n) Audit Committee Work Plan 2014/15 The Chair presented the work plan and enquired if members were happy with the content. The content of the work plan was agreed. RESOLVED: That the Audit Committee Work Plan for 2014/15 was agreed. o) Quality, Innovation, Productivity and Prevention Mr Parr presented the report to inform the AC of the current position relating to achievement of 2014-15 Quality, Innovation, Productivity and Prevention (QIPP) target and provide assurance on the process. It was noted that the schemes would be presented to the Operations Group in November which monitors performance and progress. RESOLVED: That the Audit Committee noted the achievement against the 2014/15 QIPP target for the period April 2014 to September 2014. p) Quality, Performance and Effectiveness Committee Dr Nigel Horsfield drew out key elements from the minutes from the QPEC. Minutes of the meeting held on 30th April 2014 The Audit Committee noted the minutes. Minutes of the Meeting held on 28th May 2014 The Audit Committee noted the minutes. Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 14 of 29 Minutes of the Meeting held on 25th June 2014 The Audit Committee noted the minutes. Minutes of the Meeting held on 30th July 2014 The Audit Committee noted the minutes. RESOLVED: That the Audit Committee noted the content of the minutes of the Quality, Performance and Effectiveness Committee. 5) Information Governance Steering Group Chair – Mr Roger Parr, Chief Finance Officer/Senior Information Risk Owner (SIRO) Minutes of the Meeting held on 25th November 2014 a) Information Governance (IG) Toolkit The CCG is aiming for level three on some of the requirements this year. Internal audit are visiting the CCG on 9th December 2014 for an initial view of the evidence available so far. Internal audit will then submit a report with recommendations to complete actions by the end of March 2015. b) IG Training The CCG is currently at 99% of staff having completed their annual IG training. 1 member of staff is being followed up. c) Information Security SIRO reports show that there is a good level of information security awareness within the CCG and this is reflected within spot check audit reports. d) Freedom of Information (FOI) The IG Group agreed the FOI process has improved, however, Mrs Claire Moir, Governance, Performance and Risk Manager, will be meeting with the Commissioning Support Unit to review outstanding issues. e) Privacy Impact Assessments (PIAs) and Information Sharing Agreements (ISAs) The PIA and ISA for the Accident and Emergency project is now complete and in the process of being signed off. 6) Lancashire Clinical Commissioning Group Chairs’ Network Chair – Dr Chris Clayton, Blackburn with Darwen CCG Minutes of the Meetings held on 25th September 2014 and 30th October 2014 The ratified minutes of the above meetings are attached as Appendices A, B and C. 7) Blackburn with Darwen Health and Well-being Board Chair – Councillor Mohammed Khan Minutes of the Meeting held on 8th December 2014 The approved minutes of the above meeting are attached as Appendix D but subject to the following amendment: Page 4, paragraph 5, line 3 to “and the delivery of early help for children Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 15 of 29 and families “ to be deleted and replaced with “and Transforming Lives delivery model in Blackburn with Darwen”. 8) Recommendation The Governing Body is requested to note the content of the report. Mr Iain Fletcher Head of Corporate Business 5th January 2015 Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 16 of 29 Appendix A Meeting held on Thursday 25 September 2014 Meeting room 231, Second Floor, Preston Business Centre, Watling Street Road, Fulwood, Preston PR2 8DY Present: Dr Chris Clayton (Chair) Blackburn Dr Ann Bowman – Greater Preston Dr Tony Naughton – Fylde & Wyre Dr Amanda Doyle – Blackpool In attendance: Mrs Linda Riley - LCSU Mr Carl Ashworth – LCSU Ms Samantha Nicol – Healthier Lancashire Programme (item 3) Mr Martin Clayton – Area Team (item 6) Mrs Jan Ledward - Greater Preston/Chorley & South Ribble Mr Peter Tinson – Fylde & Wyre Mr Mike Maguire – West Lancashire Mr David Bonson – Blackpool Mr Mark Youlton – East Lancashire Mrs Jill Truby – Network (minutes) 1. Welcome, apologies for absence and declarations of interests Dr Chris Clayton welcomed everyone to the meeting. Apologies for absence were received from Dr Mike Ions, Dr John Caine, Dr Gora Bangi, Dr Alex Gaw, Mrs Debbie Nixon, Mr Andrew Bennett, Ms Karen Sharrocks and Mr Andy Roach. It was noted that there was no representation from Lancashire North; therefore the meeting was not quorate. There were no declarations of interests in relation to agenda items. 2. Minutes of meeting held on 28 August 2014 Minute 2.2 Specialised Commissioning – final sentence to read “Mrs Ledward informed the group that the National Commissioning Specialised Services Task and Finish Group was meeting ………………” Minute 4 Network Governance Following sentence to be added after “A wide ranging discussion followed. Mr Maguire suggested that contribution to Lancashire collaborative schemes should be proportional to the contract financial values not per head of population wherever possible. Various opinions were expressed ……………..” Subject to the above amendments the minutes of the meeting held on 28 August 2014 were accepted as an accurate record. 3. Matters arising and action sheet The Chairman sought and obtained confirmation that the actions from the previous meeting were either complete or in hand. 4. Healthier Lancashire Dr Clayton welcomed Ms Samantha Nicol to the meeting. Dr Clayton reported that regular meetings were being held and it was noted that the next Leadership forum scheduled for 2 October would be in the format of workshops. Ms Nicol introduced herself and gave a presentation on Healthier Lancashire. Highlights of the presentation included: Background: • Historic timeline and key milestones that have been undertaken in the last 12 months. Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 17 of 29 • The case for a ‘Health and Care Strategy for Greater Lancashire’ was promoted by the Lancashire Leadership Forum throughout 2013. • Strategic workshops took place end 2013. • Followed up by a paper presented to key partners and the 3 Health & Well Being Boards. • Key work streams were set up March 2014 to establish some foundations for the programme. • Substantive Programme Director, in place from September 2014. Commitment: • Taken from the draft Strategic Framework – due to be released on 30 October 2014 This reminded members of what they have already agreed to. Progress so far: • Lancashire Leadership Forum meeting quarterly and Healthier Lancashire Executive in place • Enabling projects: o Digital Health o Listening to Lancashire o Leadership Collaboration • Operational Projects: o In-hospital o Out of Hospital o Neighbourhood Pilots o Third Sector • Sustainability Assessment Framework (SAF) • Programme Management Office in set up phase • Initial key stakeholder conversations underway System management – creating a programme • Phases and outputs • Timeline • Process for services change The Healthier Lancashire Programme will be structured into five stages • Mobilisation • Design • Implementation • Delivery • Procurement, contracting and delivery • At the end of each phase there will be a clear commitment point before moving into the next one Illustration of the process for system wide services reconfiguration: • The process for whole system reconfiguration is about ensuring recommended preferred options are based on the whole system reconfiguring, including primary care. • In phase one, mobilisation, a commitment is needed from all statutory organisations involved to work together collaboratively. This leads into the need for a robust case for change – a public facing document that creates the momentum for change. Prior to beginning the co-design of services in the new system it is vital that quality standards are set. They are another way of showing what needs to change and why and they enable the setting of priorities for action and are a way of engaging with a larger constituency. The co-design requires the right people to be together to design the possible service models and a particularly important part for the inhospital group is the work on the clinical interdependencies. This process looks at many aspects. • A vast array of options is necessary. • The process sets out the key activities, but is based on the psychology of co-design and of the need to engage people and more importantly to not close down options before it is necessary, leading to a high level of innovation and improvements. Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 18 of 29 Next steps: Governance Structure • Establish Programme, Clinical and Stakeholder Boards • Define ‘purpose’ and develop narrative and visual identify • Agree finance and resource needed • Set up PMO and put processes in place • Re-launch work streams • Collaborative Leadership – progress, incorporate ‘cultural change’ element • Develop programme plan • Agreement to mobilise General discussion ensued and it was agreed that Healthier Lancashire would become a standing item on future Network agendas and detailed information around resources would be on the October agenda. In response to a question from Mr Maguire, Ms Nicol confirmed that the programme included mental health for all residents regardless of age. 5. Collaborative Commissioning Board governance arrangements Mr Peter Tinson reported that the terms of reference had been shared and would be signed off at the first meeting of the Collaborative Commissioning Board (CCB). There was some discussion around future meeting dates and these would be agreed at the first meeting. 6. Primary care costs Further to a request at the July meeting of the Network, members received financial information relating to primary care costs split by CCG. Mr Martin Clayton attended from the area team and took questions from members relating to the information provided. It was noted that all CCGs would receive details of the models available, budgets and the various options of support. There would also be proposed models for conflict of interest and performance. It had been agreed to extend ability to change constitutions to end of December. Members agreed that it would be useful to have a model constitution. Mr Clayton took the opportunity to update the Network around the NHS England organisational alignment capability programme. Mr Clayton was thanked for attending and updating the Network. 6.1 Conflicts of interest Deferred to await national conflicts of interests policy. 7. Network governance update It was considered that the Network governance would continue as originally agreed based on the CCB. 8. Stroke update Mrs Ledward presented a stroke update. Introductory briefings will be prepared that will give people, particularly those who have not engaged as yet, time to catch up with the overall aims of the review, background context and progress to date. In addition to this early engagement process, there is further work to ensure continuing communication and consultation with CCG membership, other representative bodies, such as voluntary organisations, practice-based patient participation groups and locality forums and links to groups that are hard to reach. A detailed communications plan will be developed which will set out the basis for on-going communication and engagement between the programme, CCGs and key stakeholders including statutory bodies, provider organisations, public, patients and carers. Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 19 of 29 CSU is looking at options, numbers, travelling time etc. A GP from Blackburn with Darwen has been appointed to the clinical senate primary/secondary work stream for Lancashire. Dr Doyle agreed to share Blackpool’s work. The Network: • Noted the contents of the report 9. Individual Patient Activity Programme Board update Mrs Linda Riley updated members in relation to the current status of IPA services provided by the CSU across the Lancashire CCGs footprint. The CCGs had advised the following to be taken forward which was agreed at the Customer Forum: • The CCGs to take ownership of the IPA Programme Board with immediate effect • To secure independent external expertise to work with us to further review areas of concern • To work jointly to look at alternative options for service provision of Lancashire CCG IPA services. The CSU is keen to work with CCGs to secure the above outcomes but has so far not been able to secure CCG chair ownership to the programme Board in order to progress the above areas. All elements of the service will continue to be updated and provided through the IPA programme Board with necessary and appropriate updates to the CFO and / or Customer Forum. A detailed action plan had been put in place following the review by KPMG. Mrs Riley reported that the next scheduled meeting of the programme board is to be cancelled and used as a workshop. Members agreed that it was not about money/numbers but interfacing with the most vulnerable patients Lancashire is responsible for. Mrs Riley confirmed that in future quality indicators would be submitted to the Network. Members also received a copy of a monthly report advising on the highlights of work stream performance within the Individual Patient Activity Function of NHS Midlands and Lancashire Commissioning Support Unit. Members noted the contents of the report. 10. CSU services Members received a copy of a letter sent by Blackpool CCG on behalf of all Lancashire CCGs in relation to commissioning intentions for the CSU services in 2015/16. Representatives from each of the Lancashire CCGs had met on 5 September to obtain a collective view of their respective commissioning intentions for CSU services from April 2015. The Network was informed that this would be the only item at the next customer forum. 11. 111 Procurement Mr David Bonson gave an update around progress of NHS 111 service. CCGs were asked for their cooperation in delivering their CCGs approval to the procurement to enable implementation of the new contract before winter 2015. Item to be included on next CCB agenda. 12. CAMHS SRO Following the departure of the SRO for the CAMHS programme there was a need to consider the SRO function moving to another CCG. After discussion it was agreed in principle that Dr Ann Bowman would continue as clinical support and that Blackburn with Darwen would consult as to what was required. Dr Clayton to ask Mrs Nixon and Mr Hopley to action. 13. Minutes from other meetings Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 20 of 29 13.1 CAG The minutes of the Collaborative Arrangements Group meeting held on 9 September 2014 were noted for information. 13.2 Quality Surveillance 10/7/14 The minutes of the Quality Surveillance meeting held on 10 July 2014 were noted for information. 14. Any other business 14.1 Community Equipment Store – an update from Hilary Fordham, Lancashire North to be circulated. 15. Date of next meeting – 30 October 2014, Meeting room 1, Conference Suite, Floor 1, Preston Business Centre, Area Team/Specialised Commissioning in attendance. Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 21 of 29 Appendix B Ratified Minutes Meeting held on Thursday 30 October 2014 Meeting room 231, Second Floor, Preston Business Centre, Watling Street Road, Fulwood, Preston PR2 8DY Present: Dr Gora Bangi (Chair) Chorley and South Ribble Dr Ann Bowman – Greater Preston Dr Mike Ions – East Lancashire Dr Amanda Doyle – Blackpool Dr John Caine – West Lancashire Dr Alex Gaw – Lancashire North In attendance: Mrs Linda Riley - LCSU Miss Samantha Ruthven-Hill – LCSU Mr Declan Hadley (item 4) Mr Stewart Bond (item 4) Ms Samantha Nicol – Healthier Lancashire Programme (item 5) Mrs Jennifer Aldridge (item 9) Mrs Jean Rollinson (item 9) Mrs Alice Marquis-Carr (item 9) Mrs Jan Ledward - Greater Preston/Chorley and South Ribble Mr Mike Maguire – West Lancashire Mr David Bonson – Blackpool Mrs Debbie Nixon – Blackburn with Darwen Mrs Sarah Camplin – Fylde and Wyre Mrs Hilary Fordham – Lancashire North Mr Mark Youlton – East Lancashire Mr Gary Raphael – Blackpool Ms Karen Sharrocks – Chorley and South Ribble Ms Kathryn Chester – Chorley and South Ribble 1. Welcome, apologies for absence and declarations of interests Dr Gora Bangi welcomed everyone to the meeting. Apologies for absence were received from Dr Chris Clayton, Dr Tony Naughton, Mr Andrew Bennett, Mr Peter Tinson, Mr Carl Ashworth, Mr Iain Crossley, Mr Iain Stoddard, Mr Roger Parr, and Mr Paul Kingan. There were no declarations of interests in relation to agenda items. 2. Minutes of meeting held on 25 September 2014 Agenda item 2 (Network Governance) CCG Network minutes from 2 September 2014 was queried by Mr Mike Maguire, with reference to the contribution to Lancashire collaborative schemes being proportional to the contract financial values and not per head of population wherever possible. It was noted that a discussion had taken place but no decision made. Subject to the above amendments, the minutes of the meeting held on 25 September 2014 were accepted as an accurate record. 3. Matters arising and action sheet The Chairman sought and obtained confirmation that the actions from the previous meeting were either complete or in hand. 4. Healthier Lancashire Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 22 of 29 Dr Bangi welcomed Ms Samantha Nicol to the meeting. Ms Nicol updated members on the Healthier Lancashire Programme. Copies of the presentation had been circulated and members were asked for any comments and/or questions. Ms Nichol outlined the Healthier Lancashire process and why it is being undertaken: • Healthier Lancashire is about creating an environment across Lancashire to deal with transformation issues and barriers, work collaboratively, whilst also allowing CCGs to develop independently. • Healthier Lancashire will ensure resources are organised in a way to achieve better health outcomes. • On 27/11/2014 a document will be published that will include input and information received during Healthier Lancashire discussions. • The document will include the vision, values, principles, commitment, and scope of the Healthier Lancashire programme. • CCGs will be able to review and provide feedback on the document • The decision making process will be clearly defined within the document. Further discussions are required to confirm the leadership and decision making process for Healthier Lancashire. 5. GP IT Strategy Mr Declan Hadley and Mr Steward Bond outlined the potential areas for collaboration around digital health across the Lancashire CCGs. The proposed initiatives aim to bring together the Healthier Lancashire Digital Health Programme, the emergent CCG IT Strategies and the Informatics Work Plan of the Commissioning Support Unit. Fourteen potential areas for collaboration have been identified. CCGs were asked to prioritise the areas they wished to collaborative on. The following actions were agreed: • Approach providers and other stakeholders to establish how their priorities align • Develop a detailed proposal based on the emergent priorities • Consolidate this revised plan into the Healthier Lancashire governance structure • Link with the North West Coast AHSN to share good practice and innovation • Indicate whether they wish to collaborate on a low, medium or high level Further information was requested in order to progress this collaboration, particularly capital charges and finance issues. Some of the collaboration areas will be easier to implement than others, and it was agreed to commence these areas first. It was agreed that a financial strategy was required in order to progress the GP IT Strategy. The financial strategy should include modelling, affordability, pros and cons, what we are doing now against opportunities for the future, timelines, and mapping of the next steps. It was agreed that a more comprehensive GP IT Strategy plan should be prepared and submitted to the CCG Network meeting on 18th December. CCGs to complete template forms and return to Mr Declan Hadley by mid-November. 6. Mental Health reconfiguration Mrs Debbie Nixon verbally updated members in relation to the Mental Health Inpatient reconfiguration: • This is on track to deliver by the deadline of 2017/18 and efficiency savings will be achieved. • There is an encouraging trend of reduced out of area placements. • Delayed discharge is currently being reviewed. • The Crisis Acute Pathway is also being reviewed. • The Task Finish Group have agreed to continue with funding. Mrs Nixon will produce a paper to be submitted to the Collaborative Commissioning Board. The CCGs can then present the paper to their Governing Bodies. 7. CSU contracts for 2015/16 Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 23 of 29 Mrs Linda Riley verbally updated members in relation to CSO Contracts for 2015/16. The 2015/16 CSU contracts are being negotiated, and CCGs have been provided with pricing information. A table has been produced by service line advising of what is included and the prices. The Lead Provider Framework with prices will be ready for January 2015. However there are some uncertainties due to a number of CCGs indicating significant reductions in contracts with CSU. The impact needs to be understood and business cases developed to be considered by NHS E area team. 8. Differences between Lancashire and GM financial planning assumptions Discussion ensued around arrangements following the merger of the area teams in Lancashire and Greater Manchester and the possible consequences for Lancashire CCGs. It was agreed that the Collaborative Commissioning Board would take this forward at its meeting on 11 November in liaison with Healthier Lancashire. 9. Multi-Agency Safeguarding Hub (MASH) Mrs Jennifer Aldridge, Mrs Alice Marquis-Carr and Mrs Jean Rollinson gave a verbal presentation on the future involvement of health into Lancashire’s Multi-Agency Safeguarding Hub (MASH). The six CCGs across the Lancashire County Council footprint have been asked to consider and support a proposal for a continued health presence within the Lancashire MASH. The CCG Network was asked to receive the CCG responses to the recommendations within the paper and to agree to consider the proposal and the commissioning responsibilities to the Lancashire Commissioning Board. After general discussion members agreed that there was a need to understand the complexity of the arrangements and it was proposed and agreed to set up a task and finish group. Mrs Ledward agreed to lead this group and to bring back to the Collaborative Commissioning Board meeting a paper detailing current arrangements and proposed options going forward. 10. Minutes from other meetings 10.1 The draft minutes from the Collaborative Commissioning Board held on 15 October 2014 were noted. 11. Any other business 11.1 CAMHS SRO A paper was presented proposing that Blackburn with Darwen CCG becomes the CAMHS SRO. Blackburn with Darwen CCG is already the lead contractor for the LCFT Mental Health contract, overseeing all elements of the contract including CAMHS. The COO in BwD is also the SRO for major reconfiguration of Adult and Older Adult specialised inpatient services, and leads on the co-ordinating of the commissioning intentions and required service redesign, monitoring arrangements and transition. The commissioning of CAMHS services is supported by the CSU but ultimately accountable to current SRO (East Lancashire CCG). Due to the number of different arrangements currently within CCGs it was agreed that the CSU be tasked with incorporating all arrangements into a proposal for presenting to the CCB. It was noted that Dr A Bowman was the Network’s clinical lead for CAMHS. It was also noted that a paper re CAMHS was being considered at the Lancashire HWB. 11.2 LCA letter re CHC Rates It was established the all Lancashire CCGs had received this letter and Mrs Riley on behalf of the CSU agreed to draft a response on behalf of Lancashire. 11.3 Primary Care Co-commissioning Dr Doyle referred to an email from Mr Martin Clayton regarding preparing for co-commissioning of primary medical services. Mr Clayton had proposed that a sub-group of the CCB be set up to manage this issue going forward. Dr Bangi volunteered to Chair this group and CCGs were asked to send nominations for the group to Dr Doyle. 11.4 Telestroke Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 24 of 29 Mrs Ledward reported that following analysis of providers she would bring back a paper recommending a decision on the outcome of the negotiation of the services following the termination of the contract by North Cumbria. She advised this was an urgent issue due to the contract ending in December. 12. Date of next meeting – 27 November 2014, Meeting room 231, Floor 2, Preston Business Centre, Area Team/Specialised Commissioning in attendance. Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 25 of 29 Appendix C Meeting held on Thursday 27 November 2014, 09:00 to 12:00 Meeting room 231, Second Floor, Preston Business Centre, Watling Street Road, Fulwood, Preston PR2 8DY Present: Dr Chris Clayton (Chair) – Blackburn with Darwen Dr Ann Bowman – Greater Preston Dr Mike Ions – East Lancashire Dr John Caine – West Lancashire Dr Tony Naughton – Fylde and Wyre Mr Andrew Bennett – Lancashire North Mrs Jan Ledward – Greater Preston/Chorley and South Ribble Mr Mike Maguire – West Lancashire Mr David Bonson – Blackpool Mr Peter Tinson – Fylde and Wyre In attendance: Mrs Linda Riley - LCSU Mr Carl Ashworth - LCSU Ms Samantha Nicol – Healthier Lancashire Programme (Item 3) Mr Richard Jones – NHS England Ms Preeti Sud – NHS England (Item 2) Mr Peter Elton – NHS England (Item 2) Ms Kathryn Chester – Greater Preston/Chorley and South Ribble (Minutes) 1. Welcome, Apologies for Absence and Declarations of Interests Dr Chris Clayton welcomed everyone to the meeting. Apologies for absence were received from Dr Gora Bangi, Dr Amanda Doyle, Mrs Debbie Nixon, Ms Susan Warburton, Dr Alex Gaw, Ms Jenny Scott, and Ms Karen Sharrocks. There were no declarations of interests in relation to agenda items. 2. Respiratory Network for Lancashire Ms Preeti Sud and Mr Peter Elton gave a presentation on respiratory care in Lancashire. Specific highlights included: • Lancashire has the worst premature mortality rate for lung disease in England. • Respiratory emergency admissions feature strongly in the top 10 emergency admissions by diagnosis in Lancashire. • The average length of hospital stay for COPD in Lancashire is above the national average. • The number of COPD non elective zero day admissions in Lancashire has reduced. • In 2012/13 the Lancashire Area Team had 11,393 undiagnosed COPD cases, and 35,164 undiagnosed asthma cases. • A national respiratory strategy has been published. There are NICE guidelines for COPD and asthma. There are commissioning toolkits and other resources available, and a virtual network is being established nationally (Respiratory Futures). • Ms Sud agreed to help CCGs to take stock of the current situation and acknowledged the challenges and opportunities for improving quality of respiratory services across Lancashire. Action • CCGs to confirm their respiratory lead and provide Ms Sud with this information. 3. Healthier Lancashire Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 26 of 29 Dr Clayton welcomed Ms Samantha Nicol to the meeting. Ms Nicol updated members on the Healthier Lancashire Programme: • Healthier Lancashire was covered on the agenda at the recent Executive Group meeting. • A Healthier Lancashire Summit has recently taken place and was attended by 115 people. • The Lancashire Leadership Forum is taking place on 27 November, and the Healthier Lancashire draft Purpose Document will be presented at this meeting. • Members to review the document over the next 2 weeks, and provide feedback to Ms Nichol. An amended document will then be produced in January 2015. • The next phase of Healthier Lancashire commences on 5 February 2015. • The Purpose Document will confirm whether tasks are most suitable to be completed locally by CCGs or whether they should be completed at a Lancashire level. • Lancashire County Council Budget cuts could impact on Healthier Lancashire. • Members requested further clarity regarding organisations that are supportive of Healthier Lancashire, and those that are not supportive. 4. and 5. Primary Care Co-commissioning and Specialised Commissioning Mr Richard Jones provided an NHS England update on primary care co-commissioning and specialised commissioning: • NHS England will be announcing new operational commissioning directors on 28th November. • There will be a new appointment for the Lancashire and Greater Manchester area. • There will be a 50% reduction in VSM appointments across the North of England, and a voluntary redundancy package will be available. • The new roles will go live at the end of January 2015. • CCGs will be expected to take on some extra roles from NHS England. • NHS England will monitor the performance of the new system and provide assurance. Should any failure be identified, NHS England will be able to intervene and use its’ powers. • NHS England’s 5 year forward view is to encourage local systems to build on existing work, and co-commissioning to ensure the focus for Lancashire is not lost. • Some specialised commissioning is returning to CCGs as part of Tier 3 services. • These include neurology outpatients and referrals, renal dialysis, bariatric surgery and specialised wheelchairs. • CCGs will be advised as to who is providing these services, and co-commissioning will commence in 2015. • A national group has been created to review the budgets for specialised commissioning. • The implementation of specialised commissioning services will be discussed at the CCB meeting, and then discussed at the Network on 18th December. • Specialised Commissioning Boards to be set up for Tiers 2 and 3 by February 2015, and South Cumbria to be included in the planning. Actions • Members to identify any statutory actions that are required in order to implement specialised commissioning. • Co-commissioning Board to pick up the issue of specialised commissioning and raise significant issues for the Network to consider. 6. Minutes of CCG Network Meeting Held on 30 October 2014 Mrs Linda Riley advised of an error within agenda item 7 on page 2 of the minutes. This should read as the Lead Provider Framework with prices will be ready for January 2015 and not September 2015. Subject to the above amendments, the minutes of the meeting held on 30 October 2014 were accepted as an accurate record. 7. Matters Arising and Action Sheet Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 27 of 29 The Chairman sought and obtained confirmation that the actions from the previous meeting were either complete or in hand. 8. IPA Update Mrs Linda Riley provided an update on IPA: In July 2014 CCGs made three requests in relation to IPA and CHC: • CCGs to take ownership and chair the IPA Boards. • Systems to be reviewed and CCGs to be given assurance. • To jointly look at the alternative models of future care provision. Following a meeting on 1 November with CCGs, 5 work streams have been identified and 2 representatives from each CCG have been agreed. A formal report from Ian Fletcher will be presented to the Network on 18 December. The concept of a clinical lead for IPA was further discussed and the specific requirements will be considered by the Network. 9. Minutes from Other Meetings The draft minutes from the Collaborative Commissioning Board held on 11 November 2014 were noted. AB drew the attention of the meeting to the item 9, Transforming Community Equipment Services, and the resolution made by the CCB: ‘The TCES programme has been developed as a Lancashire-wide procurement of services. In addition to the 6 CCGs within the programme, LCC is a key party to the process. Through the CAG there has been an established agreement with ELCCG to request a variant bid, in addition to the Lancashire-wide bid. CCB is asked to support a continuation of the procurement process and the inclusion of the EL variant bid. ELCCG is asked to participate fully in the tender evaluation process and work with all partners to secure the best tender outcome for all CCGs and LCC.’ It was noted that East Lancashire CCG had subsequently agreed this CCB resolution. On this basis, JL agreed on behalf of GP/C&SR CCGs that the procurement could now progress to PQQ. AB reported that the programme will progress to tender before Christmas. 10. Any Other Business 10.1 IFA and Non-Commissioned Procedures Policies Dr Ann Bowman advised that individual CCGs have been writing their own policies rather than using Lancashire policies. The reasons for this needed to be discussed, as the CCG Network had previously agreed on joint policies. Mrs Jan Ledward advised that a meeting had been organised to discuss this matter but only Chorley and South Ribble and Greater Preston attended this. The risk of not having any policies in place had been identified, and processes were put in place due to the old policies being out of date. Eleven draft policies written by Karen Slade have been approved, and it was suggested that these are adopted across Lancashire. It was agreed that a Lancashire approach to policy development is required. 10.2 Stroke Update Mrs Jan Ledward provided a stroke update: • Following a request for expressions of interest, two proposals have been received from Blackpool CCG and East Lancashire CCG. • Both CCGs have advised that the cost to continue with the service will be over £100,000. Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 28 of 29 • • • Both CCGs have been asked to justify this cost. East Lancashire has responded, advising that there will be an improvement in quality. Blackpool is yet to respond, but needs to do so by Monday 1 December 2014. Rationale will be provided to support the decision when a CCG is chosen to provide the stroke service. There are CCGs who have not replied to confirm their agreement to the stroke service specification. These CCGs will be emailed directly by Mrs Ledward. Action Mrs Ledward to email CCGs who have not yet confirmed their agreement to the stroke service specification. 10.3 Neurology and Dermatology Mrs Ledward presented a letter from Salford CCG advising that waiting times for neurology, spinal surgery and dermatology at Salford Royal Foundation Trust are breaching the RTT standards for both admitted and non-admitted. The letter requests that CCGs in Lancashire, Mersey and West Cheshire support GP practices to consider Preston and Walton Neurology services before electing to refer to SRFT. Action Mrs Ledward to prepare a letter to be sent to the specialised commissioning team for advice regarding this matter. 11. Date of Next Meeting – 18 December 2014, 09:00 to 12:30, Meeting Room 1, Floor 1, Preston Business Centre. Governing Body Sub-Committees and Groups’ Summary – 14th January 2015 Page 29 of 29 Appendix D
© Copyright 2026