Digestive filled
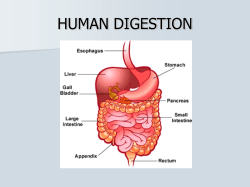
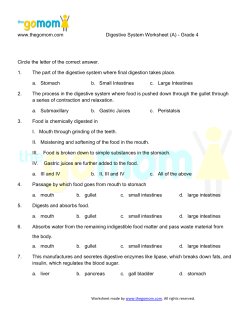
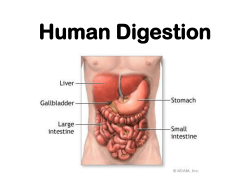
I. Processes overview 1) Ingestion Taking in food 2) Movement Transporting food material and waste down the digestive tract 3) Digestion Breaking food material down into smaller parts: Two processes Mechanical Breaking food down using physical processes: chewing and mixing Chemical Enzymes break food macromolecules down into small subunits Starch into glucose; proteins into amino acids. 4) Absorption The subunits are absorbed into the blood stream 5) Defecation Waste material is eliminated from the body. II. Organization 1) Organs of the gastrointestinal (GI) tract Pharynx, esophagus, stomach, Small intestine, large intestine 2) Accessory structures Teeth, tongue, salivary glands, liver, gallbladder, pancreas. III. GI tissue Mucosa A mucous membrane that lines the lumen of the digestive tract Epithelium ! Most of the length simple columnar epithelium. ! Oral and anal ends: nonkeratinzed stratified squamous. lamina propria ! This is a layer of CT under the epithelium muscularis mucosae ! Under the lamina: a thin layer of smooth muscle plicae ! Folds of the mucosa ! Increases surface area ! Allows the digestive organs to expand. III. GI tissue Submucosa connective tissue Areolar (loose) blood vessels and lymphatics Glands ! Submucosal glands ! Secrete enzymes and buffers Muscularis externa ! Two layers: ! Outer longitudinal ! Inner circular Serosa adventitia ! Ootermost layer ! Also called the viseceral peritoneum. III. GI tissue Visceral peritoneum Is the inner membrane that covers organs in the abdominal cavity. Forms part of the … Peritoneum ! The serous membrane of the abdominal cavity; similar to the pericardial and pleural membranes. Parietal Peritoneum is the outer membrane which lines the cavity. Peritoneal cavity The potential space between the two membranes; filled with a serous fluid. III. GI tissue Extensions Of the peritoneum extend throughout the abdominal cavity Mesentery Double-layered folds of the peritoneum. Bind the organs together. Anchor them to the posterior wall Falciform and coronary ligaments Attaches the liver to the anterior abdomen and the diaphragm Lesser and greater omentum The former: suspends the stomach from the liver. Latter: hangs down in front of the intestines. IV-V. Mouth and tongue Oral cavity Entry into the digestive system. Consists of accessory organs that start digestion. Teeth for mastication Tongue to manipulate food and generate speech. Also taste buds are located here. Salivary glands secrete into the oral cavity. Place where swallowing reflex is initiated. IV-V. Mouth and tongue Lingual frenulum ! Attaches the tongue to the floor of the mouth. Papillae Bumps of mucosal and CT on dorsal surface of the tongue. Give it rough texture. Manipulate food Salivary glands Produce saliva Three sets: Parotid ! Largest: Ant/inf to ears Submandibular ! Medial surface of the mandible. Sublingual ! Under the floor of the mouth. IV-V. Mouth and tongue Saliva ! Composition: ! ! 98% water ! ! ions: Na+, Cl-, bicarbonate ! ! mucin ( protein, lubrication) ! ! salivary amylase ! Enzyme which breaks down starch into maltose (a disaccharide) Functions: 1) Dissolves food chemicals 2) Moistens and lubricates food 3) Carbohydrate digestion starts here IV-V. Mouth and tongue Deglutition Or the swallowing reflex. Bolus A mass of chewed food mixed with saliva. Deglutition starts with… Buccal stage Or voluntary stage. The tongue moves the bolus towards the oropharynx. Pharyngeal stage The bolus in the pharynx triggers a series of reflexive contractions. Forces the bolus into the esophagus Esophageal stage Contractions carry the bolus down the esophagus. The esophageal sphincter at the distal end opens. VI. Esophagus Muscular tube: 2.5x25 cm Extends from the pharynx to the stomach Function: transport a bolus to the stomach. Mucosa Similar to the mucosa describe before. Muscularis layer is very prominent. Peristalsis Involuntary waves of smooth muscle contraction. Moves a bolus through the GI tract. Esophageal sphincter Located: distal esophagus, just before stomach. Constricts to prevent back flow of stomach contents. If the sphincter fails, backflow or acid reflux occurs. Also called… Heartburn. Irritation of esophageal lining. VII. Stomach Function. 1)! Food storage 2)! Chyme production 3)! Protein digestion 4)! Mucus production 5)! Absorption of nutrients (very little) Subdivisions. 1)! Fundus Bulges above the entrance of the esophagus. 2)! Cardia Around the opening of the esophagus. 3)! Body The open area below the fundus: about 2/3 of the stomach volume. Lesser curvature- concave medial border. Greater curvature- convex lateral border 4)! Pyloric region Narrow region distal to the body Pyloric sphincter- between the duodenum and the pyloric region VII. Stomach Adaptations of the stomach for digestion. 1)! Rugae Prominent longitudinal folds of the stomach mucosa. Easily seen when the stomach is empty. Allows the stomach to distend with food. 2)! Gastric pits (3 million) Openings to collections of gastric glands (15 million). Allow gastric juice to enter the stomach lumen. VII. Stomach Gastric glands contain 1)! Parietal cells secrete Instrisic factor Aids in vitamin B12 absorption HCl- hydrochloric acid pH ~2 For break down of cells (bacteria, plant). 2)! Enteroendocrine cells or G cells Produce hormones which regulate gastric function such as gastrin. 3)! Chief cells Produce pepsinogen Precursor to pepsin, a proteolytic (breaks down proteins) enzyme VII. Stomach Gastric juice Made by gastric glands. Consists of mucous, HCl, water, pepsinogen, and intrinsic factor. You make about 1500 ml/day Gastric juice mixed with food is called acidic chyme. Infants Also have the enzymes rennin and gastric lipase in gastric juice. Important for the digestion of milk proteins and milk fat, respectively. VII. Stomach Regulation of gastric function Cephalic phase (“head” phase) ANS is stimulated by thoughts of food or smells, time of day. Stimulates the release of gastric juice. Prepare the stomach for the arrival of food. Also release of the hormone gastrin which stimulates: chief and parietal cells Contractions in the stomach wall VII. Stomach Gastric phase (“stomach” phase) When food arrives, stretches the stomach. Stimulates release of gastrin and gastric juice. Also triggers “mixing waves”; contractions of the stomach wall to mix food and gastric juice. Also increases intestinal motility (movement.) Start protein digestion. VII. Stomach Intestinal phase Gastric emptying. Acidic chyme is passed into the first part of small intestine (duodenum.) Only small amounts are released. Distention of the duodenum releases CCK which affects the liver and gallbladder. VII. Stomach Regulatory functions are inhibitory to the stomach. Called enterogastric reflexes. Acidic chyme distends the duodenum Inhibits gastrin production Reflexes shutdown gastric activity until the chyme passes further down the small intestine. Contractions in the stomach (mixing waves) are inhibited. Gives time for the duodenum to deal with the acidic chyme. Several hormone are released by the duodenum when chyme arrives from the stomach. ! Secretin and CCK (cholecystokinin) ! These affect the pancreas and liver, respectively. ! More on these later. VII. Stomach Gastric activity. Vomiting Or reverse peristalsis. The stomach lining becomes overly irritated strong contractions occur Chyme is propelled in the opposite direction, up the esophagus. Function: to remove irritant from the stomach. Absorption Of nutrients is not a major function. Stomach absorbs Water Alcohol Aspirin Some ions, only if they are severely depleted VIII. Pancreas The pancreas is a heterocrine organ Has 2 Functions: 1)! Endocrine: release of the hormones insulin and glucagon 2)! Exocrine: the formation of pancreatic juice, which contains digestive enzymes, water, bicarbonate and other substances. VIII. Pancreas Gross anatomy Location: inf/post to stomach Near the duodenum (proximal part of the small intestine) Pancreatic duct- leads from the pancreas towards the duodenum. Hepatopancreatic duct or ampulla is formed by a union of the pancreatic duct with the common bile duct. This common duct empties into the duodenum. VIII. Pancreas Control of pancreatic juice •" Acidic chyme (from the stomach) enters the duodenum •" Triggers the release of secretin (hormone) from the duodenum •" Secretin stimulates the pancreas to release pancreatic juice. •" The secretion enters the duodenum •" Starts to digest the chyme •" Acidic chyme also stimulates the duodenum to release cholecystokinin (CCK). VIII. Pancreas Pancreatic juice contains many pancreatic enzymes which digest different food materials. •" Alpha-amylase Breaks down starch to disaccharides (2 glucose molecules) •" Pancreatic lipase Breaks down fat into fatty acids and glycerol •" Nucleases Digest DNA and RNA molecules VIII. Pancreas Proteinases or proteolytic enzymes Trypsin, chymotrypsin, carboxypeptidase, elastase All break down proteins into amino acids. •" Proezymes Proteinases are released in an inactive form a called proenzymes. Trypsinogen, chymotrypsinogen, procarboxypeptidase, proelastase These are inactive, otherwise they would digest pancreatic cells. •" Enterokinase Released by the epithelium of the duodenum. Converts the proenzyme trypsinogen into trypsin. Trypsin converts the other proenzymes into their active forms. •" Active enzymes require an alkaline environment. Pancreatic enzymes cannot function in acidic chyme (~pH 2.) Bicarbonate of pancreatic juice converts the acidic chyme alkaline chyme (~pH 8.) Enzymes can function normally. IX. Liver The liver has three major functions 1)! Metabolic regulation Carbohydrate metabolism Helps to maintain proper blood glucose levels. Lipid metabolism- maintain blood fatty acid, triglycerides and cholesterol Amino acid metabolism-removes extra amino acids Detoxifies blood Vitamin and mineral storage 2)! Hematological function Makes plasma proteins Removes hormones Removes antibodies Removal of bilirubin 3)! Bile production IX. Liver Synthesis and production of bile Bile consists of Water Bilirubin- made from the breakdown of the heme- gives bile it’s green color. Bile salts- a collection of lipids " These lipids (some derived from cholesterol) are important in making fats soluble- a process called…emulsification. ! This processes causes large fat droplets to break into tiny particles- makes it easier for lipases to break down fat. ! Without emulsification fats are difficult to digest. IX. Liver Gross anatomy Location: right hypochondriac and epigastric region Largest visceral organ Two major lobes (right and left) divided by the falciform ligament. Porta hepatis (“doorway to the liver”) Located on the posterior surface. The site where the hepatic artery and the hepatic portal vein connect to the liver. Gallbladder attaches here. IX. Liver Gallbladder Bile passes through the hepatic ducts, common bile duct, into the cystic duct, into the gallbladder. Bile is stored until needed, when it is passed out through the cystic duct, common bile duct and into the duodenum. IX. Liver Functional unit of the liver Is called a lobule, which consists of: Hepatocytes- liver cells, regulate circulating nutrients/waste levels in the blood. The vessels that supply and the ducts that drain the lobules enter at a site called the portal area. This consists of 1.! The portal vein; a branch of the hepatic portal vein. This carries nutrient and toxic laden blood from the intestinal tract. 2. Hepatic artery, which supplies O2 to the hepatocytes. 3. Bile duct tributaries which carry bile into the main bile duct. IX. Liver Sinusoids of the liver carry the blood from the portal veins slowly past the hepatocytes. The blood is processed and then passed into the central vein. This leads to the hepatic veins and then into the inferior vena cava. The waste material and bile is passed into bile duct tributaries, then into the bile duct. The liver makes about 1 lt of bile per day. X. Gall bladder Functions 1.! Bile storage: about 40-80 ml 2.! Bile modification Most of the water in bile is removed. Bile becomes concentrated Location Post/inf to the liver X. Gall bladder CCK in th blood causes the following: •" The gallbladder to contract •" The biliary (hepatopancreatic) sphincter to open •" This forces bile into the duodenum Fat droplets becomes emulsified by bile salts. ! Bile helps fat digestion. X. Gall bladder Gallstones (biliary calculi) Caused by the deposits of cholesterol and/or bile salts in the gallbladder and ducts. May cause cholecystitis- inflammation of the gallbladder . If the stones are large or numerous enough they can block the bile duct. This may cause … Jaundice (obstructive) Where the bile backs up into the liver and bilirubin can’t be removed from the blood. This builds up and causes a discoloration of the skin and other tissues. Cholecystitis and the 4 Fs ! Female ! Fair ! Forty ! Overweight XI. The Small intestine Anatomy Consists of 1.! Duodenum 2.! Jejunum 3.! Ileum Extends from the… Pyloric sphincter Distal end of the stomach, to the… Ileocecal valve Entrance to the large intestine 2.5 cm by 5-7 m Function: most of digestion and absorption of nutrients occurs here. XI. The Small intestine 1.! Duodenum Shortest: 25-30cm in length Function: Most of digestion is initiated here Submucosal glands Are prominent: provide mucus to protect the intestinal wall from acid. Plicae Large, circular folds of the mucus membrane. Extend around the lumen. Increase surface area nd allows distension. Villi Millions of finger like projections (0.2 - 1.0 mm). Extend from the mucosa. Greatly inc surface area. XI. The Small intestine Lacteals Are found w/I each villus. Consist of a capillary network and a lymph vessel Chylomicrons Droplets of lipid molecules from fat digestion. Found in the lymph fluid of the lacteal. Transports fat around the body. Intestinal Crypts or glands Collections of cells between the villi within the mucosa. Secrete enzymes and hormones. Such as Enterokinase (enzyme) and secretin and CCK (hormones): Basic function Produce intestinal juice. starts protein digestion (see pancreas and enterokinase) Increase digestiive secretion and motility (secretin and CCK) XI. The Small intestine 2. Jejnum Second segment. 1-1.5 m Larger plicae; lots of surface area. Most of nutrient absorption occurs here and in the next segment. 3. Ileum Last part: 2-2.5 m long. Intestinal secretions or juice Consist of water and enzymes. These secretions combine with pancreatic juice to complete digestion. Example: ! lactase, breaks down milk sugar lactose into monosaccharides. Intestinal lipases, amylases, peptidases. XI. The Small intestine Hormones and CNS stimulate secretions Cephalic phase (CNS/ANS) triggers gastric secretions. Hormones such as gastrin (from stomach), secretin and CCK (from duodenum) regulate their target organs. Stomach, pancreas and liver, respectively. Duodenal ulcers The lining of the duodenum is eroded by too much acid. Pyloric valve may not work properly; lets too much chyme in. Bicarb from the pancreas can’t neutralize the acid. XI. The Small intestine Intestinal movements Peristaltic movements; moves a bolus more distally. Gastroenteric reflex (stomach/intestine) Food arriving in the stomach triggers intestinal movements. This moves chyme down the intestinal tract. Gastroileal reflex Opens the ileocecal valve. Allows feces to enter the large intestine. Both reflexes speed up movement of material distally in the intestine. 80% of digestion occurs in the small intestine. XII. Large intestine Functions 1.! Absorbs 80-90% of the water/ electrolytes from the chyme. 2.! Absorbs vitamins: K, riboflavin, thiamin. 3.! Produces feces Large intestine extends from… The ileocecal valve to the anus. Dimensions: 7.5 cm x 1.5 m XII. Large intestine Major parts Cecum; ascending, transverse and descending colon; rectum. 1.! Cecum Pouch below the level of the ileocecal valve. Haustre: bulging sacs caused by the contraction of bands of smooth muscle Ileocecal sphincter: a valve that regulates the flow of chyme from the ileum into the large intestine. Appendix: vestigial organ; blind ended sac filled with lymphoid tissue. Appendicitis: inflammation of the appendix. XII. Large intestine 2. Colon Ascending colon: passes superiorly from the cecum. Right colic flexture is where the colon turns into… Transverse colon: crosses the abdomen to the left side. At the … Left colic flexture the colon turn downward into the… Descending colon Sigmoid colon: is formed when the descending colon makes an s-shaped turn before passes into the rectum. XII. Large intestine 3) Rectum Last 12-13 cm of the digestive tract. Ends at the anal canal and opens to the exterior at the anus. Muscles of the rectum At the distal end of the rectum are two sets of muscles. Internal anal sphincter: smooth muscle, involuntary External anal sphincter: skeletal muscle, voluntary XII. Large intestine Colon wall No villi or plicae. Reduced surface area. Intestinal gland Produce no digestive enzymes or hormones. Only mucus. Colonic movements Both gastroenetric and gastroileal reflexes causes contraction to occur in the large intestine. These strong smooth muscle contractions, called… Mass movements, move feces towards the rectum and trigger the defecation reflex. XII. Large intestine Feces Large intestine excretes waste as feces. Composition 75-80% water Solid material ! Bacteria ! Organic and inorganic residues ! Cell debris ! Roughage (fiber) Constipation When feces has too little water and bulk. Difficult to trigger the defection reflex. Diarrhea When feces has too much water and bulk. Triggers a string defection reflex. Cholera toxin Stimulates intestinal motility and reduces the absorption of water in the large intestine. This creates large amounts of very watery feces and severe water loss. Can be lethal if not treated quickly. XII. Large intestine Defecation reflex. The arrival of feces in the rectum triggers a reflex. There are two feedback loops 1. Stretch Distension of the rectal wall by the feces. Stimulates smooth muscle contractions in the rectum. Moves feces towards the anus. 2. ANS Triggers mass movements to push feces from the descending and sigmoid colon into the rectum. Internal anal sphincter (involuntary) opens External anal sphincter (voluntary) closes Requires conscious effort to open the ext. anal sphincter. Val salva manuver " “Straining at the stool” !
© Copyright 2026