How to Recognize and Manage Flea Allergy Dermatitis?
How to Recognize and Manage Flea Allergy Dermatitis?
Ian Spiegel, VMD, MHS, DACVD
Veterinary Specialty and Emergency Center
Levittown, PA
Ectoparasites cause pruritus: irritation and mechanical damage allergenic substances: saliva, feces, or exoskeletons;
hypersensitivity/allergic reaction
Background (fleas)
•
Fleas are wingless arthropods that feed on/infest the hair coats of mammals and the plumage of birds. There are over
2,200 species and subspecies distributed worldwide, with at least 95% known to parasitize mammals.
•
History of about 60 million years (found on pre-historic mammals).
•
Fleas are the most common external parasite of companion animals. Fleas are complete metamorphic insects, having
developmental stages consisting of eggs, larvae, pupae, and adults (1-5mm).
•
Flea allergy dermatitis (FAD) is the most common skin disease of cats and dogs. The underlying cause is a
hypersensitivity to the saliva of fleas (Flea Bite Hypersensitivity).
•
In several regions of the U.S.A and worldwide, FAD is the most common canine disease!
•
Aside from FAD, fleas can cause iron deficiency anemia/blood loss (young animals), tissue/hide damage, peripheral
eosinophilia, serve as intermediate hosts (i.e. Dipylidium caninum-fleas harbor cysticercoids), and serve as vectors for
several disease agents (some are zoonotic/public health concern) and a clinically insignificant filarial parasite
(Dipetalonema reconditum).
•
In geographic regions where there are no fleas (low humidity and/or high elevations (>5,000 ft) i.e. Denver, Lake
Tahoe, Las Vegas, etc.), atopic dermatitis (AD) is the most common skin disease of canine dermatologic patients.
Ctenocephalides felis felis (Cat Flea)
•
#1 flea infesting BOTH (97%) cats and (92%) dogs.
•
Readily attack humans and/or other mammals if desired host is absent. Cat fleas are known to infest >50 different hosts
worldwide. Aside from canines and felines, in North America, the other commonly infested animals include raccoons,
opossums, ferrets, etc.
•
Moves freely through the hair coat.
•
Intermediate Host: Diplydium caninum******
•
Potential Vectors:
o FeLV: FeLV RNA in vitro and probably also in vivo (Vobis, 2003). “Feline Leukemia Virus”
o Bartonella henselae: Can persist in flea feces in the environment for at least 3 days and can multiply in the cat
flea (Finkelstein et al, 2002). “Cat Scratch Disease”
o Mycoplasma haemofelis (formerly Haemobartonella felis): a parasite that affects the outer surface of feline
red blood cells Feline Infectious Anemia (Hemobartonellosis)******; RULE OUT in ANEMIC CATS (A
good thing to know!).
Ctenocephalides canis
(Dog Flea)
•
#2 flea infesting dogs and cats in the U.S.A
•
More common in the United Kingdom (#1 in Ireland and Greece).
•
Readily attack humans and/or other mammals if desired host is absent. When raised on cats, they do NOT develop past
the first larval stages.
•
Moves freely through the hair coat.
•
Intermediate Host: Diplydium caninum
Flea life cycle
•
Developmental cycle includes egg, larva, pupa, and adult
stages. The metamorphosis is complete (holometabolous).
•
Variable length of the cycle (12 - 190+ days) depending upon
environmental conditions
•
Under conditions of 75F and 78% relative humidity, the
developmental cycle usually varies from 16 to 26 days
depending on the insect's gender. The average is 21 days.
•
At low altitudes and ideal temperature and humidity, the
developmental cycle has taken as little as 12 days.
•
•
Dryness and high heat, very high humidity concurrent with high temperature, very wet conditions (drowns the larvae),
or extreme cold is not good for the fleas, prolonging the life cycle and thus being deleterious to larvae.
Flea infestations usually originate from the environment and not from specific contact with an infested/carrier host.
This is important in the prevention of flea-related disease/conditions.
Eggs
•
•
•
•
•
•
Larvae
•
•
•
•
•
•
•
Pupae
•
•
•
•
•
•
•
•
Adults
•
•
•
•
Smooth pearly white, and oval with rounded ends. The eggs are NOT sticky (i.e. easily fall off the host) and average
about 0.5 millimeters in length.
Eggs are laid on the host, 24-36 hours after the female flea takes a blood meal.
About 70% of the eggs fall from the hair coat within 8 hours and can be distributed any place the host has access.
Hatching occurs on or off the host but the larval development CANNOT proceed at the mammalian body temperature.
Hatching usually occurs within 1 to 10 days depending upon ambient temperature and humidity.
The larvae escape the egg shell (chorion) by using a “hatching spine” or “egg tooth” to break-out.
Larval development MUST take place off the host (mammalian temperature is too high).
Larvae are small (2 - 5 mm), slender, worm-shaped, yellow-white to brown, segmented, and sparsely covered with tufts
of “hairs” (setae/bristles). The free-living larvae are active and feed on organic debris, such as adult flea feces (“flea
dirt”), which leads to blood in the gut being noticed.
The mouth parts of larvae are mandibulate, thus allowing for the feeding on particulate matter in the environment (i.e.
bedding, corners, carpet, crevices, cracks in wood, etc.).
Larval stages last 5 to 11 days depending on the availability of food and climate.
Molting: There are 2 molts with a total of 3 larval stages (instars).
Larvae are negatively phototactic (avoid direct sunlight) and positively geotactic (actively move deep in carpet fibers
where most treatments fail to contact).
Flea larvae are EXTREMELY SUSCEPTIBLE to heat and desiccation. Not likely to survive outdoors in shade-free
areas – relative humidity of <33%-50% or >95% and/or temperature >95oF or <37.4 oF is lethal to larvae.
Occurs within a cocoon that was spun by the 3rd (final) larval instar. The cocoon is ovoid, 0.5 cm in length, whitish,
and composed of loosely spun silk.
These are sticky (unlike eggs). The stickiness allows it to become coated with particles from the surrounding
environment, this providing better camouflaging.
Pupation lasts for about 8 to 9 days on average, but can be prolonged for up to 174 days (6 months). The pre-emerged
adult flea that waits inside the cozy cocoon, waits for the ideal conditions (i.e. 80% relative humidity and 80o F)
Reports of fleas biting people after extended absences from a home (i.e. summer vacation home) can be explained by (2)
common reasons:
Potential for a prolonged pupation with development/emerging when stimulated.
Infestation of the house (attic, basement, crawl spaces) by raccoons, opossums or feral cats.
Proper stimulation for adults to expupate (emerge) from the dormant stage in the cocoon include:
o physical pressure
o vibrations
o carbon dioxide
o lactic acid
o heat
The pupal phase is the MOST DIFFICULT PHASE TO ELIMINATE with pesticides (“pupal window”). Of all the
immature stages, the quiescent pupae are the MOST RESISTANT to desiccation.
Shortly after emergence (recall that the adult flea can remain quiescent in the cocoon), adult fleas search for a desired
host (not strictly host specific).
Attraction stimuli include:
o body heat
o exhaled carbon dioxide
o air currents
o changes in light intensity
o host movements
Adult fleas are positively phototactic and negatively geotactic (opposite of the larvae).
Survival of newly emerged fleas without blood meal is limited. Newly emerged adult fleas that are unsuccessful at
seeking out a host, usually die within 12 days, but often much sooner.
•
None of the stages of the life cycle (egg, larva, pupa, or adult) have the capacity to survive exposure to <3°C (37.4°F)
for several consecutive days. However, cat fleas are known to survive cold winters (i.e. northern temperate climates) as
adult fleas on dogs/cats without proper preventative measures or on small wild mammals (i.e. raccoons, opossums, feral
cats) in the urban/suburban environments. Each flea can consume about 13.6 µL of blood daily. Female fleas consume
(blood) approximately 15 times their body weight daily (1 ml of blood can be removed by 75 fleas daily). Male fleas
consume (blood) approximately 5 times their body weight daily. The majority of the blood consumed is released as
partially digested feces that serve as essential nutrients for flea larvae (“flea dirt”). Feeding and mating occur within 824 hours and egg-laying can occur about 24-36 hours after the initial blood meal. Cat fleas have a loose association
with their host, meaning they move freely through the hair coat (unlike the “stick tight flea” of poultry which have a
long-term association with the skin surface). Once on a host, cat fleas prefer to become permanent ectoparasites and
live their entire lives on one host. Many adult fleas are removed by the animal's grooming activity (i.e. many are
swallowed, especially by cats). Thus, fleas do not generally leave on their own accord.
Egg production (female)
•
Peak: 40 - 50 eggs/day
•
Average: average for 21 day cycle is 20 eggs/day (if 50% are female, then infestation of > 20,000 adults and 160,000
pre-adult forms in just 60 days)
•
Total: +/- 2,000 eggs/flea in just 60 days! (The natural life expectancy is >100 days; but much shorter with
intervention.). Adults are responsible for transmission of disease, hypersensitivity/FAD, potential anemia, tissue
damage, and annoyance/irritation. The mouthparts of adults are suctorial/piercing, thus allowing blood meals.
Fleas & flea allergy dermatitis: diagnosis of flea allergy dermatitis/flea bite hypersensitivity
Background information
•
#1 dermatologic disease of domestic dogs in the USA.
•
Most common in warmer seasons (summer in the USA).
•
Up to 50% of dogs with fleas experience flea bite hypersensitivity.
Patient history
•
Pruritus of increasing intensity (PRURITUS is very common.)
•
Initially may be seasonal
•
Can be year-round contingent on environment
•
Licking, chewing, excessive grooming (associated with the pruritus)
•
Canine: especially rear half of the body: dorsal lumbosacral area, groin, etc.
•
Feline: generalized (often back and facial area) (removes many fleas)
•
Feet/Ears: If there is pedal pruritus or otitis externa, consider the presence of a different hypersensitivity (i.e. food +/atopy) in addition to, or in place of, FAD.
•
Increased pruritus or appearance of pruritus after new cat, new dog, move to a new house, stay at kennel, etc.
•
ONE DOES NOT NEED TO SEE A SINGLE FLEA! The most common debate with the client often revolves around
this phenomenon. At least 15% of dogs with FAD do not have evidence of fleas and hypersensitive cats (aside from
increased grooming) are thought to produce an unknown factor that leads to the production of fewer flea eggs.
•
Review the flea control with the clients:
•
What products are used (oral, topical, homeopathic, OTC, Rx, etc.)?; Are the products used properly?; Do the dogs
swim often?; How often are the pets bathed?; Environment?; Other animals in the household/environment (clinical
signs, products used on ALL animals)?- other animals may be “carriers”; Previous years? (signs often get worse each
year)
Signalment
•
Gender: No sex and breed predisposition (dogs, cats)
•
Age: Development of the disease at any age, but usually between 10 months to 5 years (as young as 4 months).
•
Young dogs may have clinical signs that present almost identical to sarcoptic mange (widespread papular and intensely
pruritic dermatitis).
•
Fleas and Flea Feces – may not be seen if animal recently bathed
•
Direct observation
•
Flea combing (Usually a good idea to make a part of a routine exam.)
•
In flea allergic animals, common to “see no fleas” on the exam.
•
They are hypersensitive- one bite may lead to an allergic reaction.
•
They are very pruritic- excessive grooming (removal of the evidence).
•
"Spot test"
•
•
Collection of suspected flea feces (comma shaped) on white paper.Add water & red staining of paper (rehydrated blood“flea dirt”)
Not always found, but when it is detected, show the client!
Physical/dermatological examination and differential diagnosis – dogs and cats
Dogs
Lesion
Dorsal caudal lumbosacral region (lowerDistribution
back)- “waist disease” or “racing stripe
Lesion Type
Other Findings
Common
Differential
Diagnosis
Cats
dermatitis” because lesions in caudal area
+/- flank
Tail head & Perineum
Caudal medial thighs
Abdominal (umbilical fold regionespecially males)
Multi-focal crusted papules (component of
“feline miliary dermatitis”)
Generalized (can have the “racing stripe
dermatitis” pattern)
“Collar” pattern (around the neck)- often
includes the head)
Back (along the entire back extending to
the neck/face)
Generalized (often spares the head)Papule (primary eruption)
Crusting (serous to hemorrhagic)
Scaling and Alopecia
Excoriations (pyotraumatic dermatitis or
acute moist dermatitis= “hot spots”)
Hyperpigmentation
Lichenification
Fibropruritic nodules (uncommon, usually
in the dorsolumbosacral region of dogs with
chronic lichenified FAD; multiple, firm,
alopecic nodules (0.5-2 cm); seen in dogs
usually > 8 years; DDX: neoplasia)
Secondary bacterial pyoderma (common)surface, superficial, and deep.
Pruritus (especially caudal)
History & Clinical Presentation
Atopy**
Food Allergy**
Sarcoptic Mange
Other Ectoparasites: Pediculosis,
Demodicosis, Cheyletiellosis
Bacterial Folliculitis +/- Malassezia
Dermatitis (commonly associated)
Other: Auto-immune/Immune-Mediated
Disease, Neoplasia (older animals), GI
Parasite Hypersensitivity (rare)
Crusted-papules
Scaling (“exfoliative dermatitis”)
Excoriations
Erythema
Feline self-induced alopecia ("Symmetric
Alopecia") +/- actual dermatitis
(sometimes only this)
Pigment changes (multifocal melenotic
macules)
Secondary bacterial pyoderma
Feline Eosinophilic Diseases:
Eosinophilic Plaque
#1 with FAD
Eosinophilic Indolent Ulcer
Eosinophilic Granuloma
Eosinophilic Folliculitis (rare)
Pruritus (generalized)
History & Clinical Presentation
+/- Peripheral lymphadenopathy
Other External Parasites:
Cheyletiellosis, Notoedres (Head mange),
Pediculosis: Felicola subrostratua,
Trombiculosis (Chiggers), Otodectic
Mange
Fungal: Dermatophytosis
Other Allergies: Food Allergy or Atopy
and Drug Reaction
Other: Auto-immune/Immune-Mediated
Disease, Idiopathic Miliary Dermatitis,
Bacterial Folliculitis, GI Parasite
Hypersensitivity, Biotin Deficiency, Fatty
Acid Deficiency
Saliva (antigens)
•
The “complete” antigens are polypeptides, amino acids, aromatic compounds, and fluorescent materials in the saliva of
fleas.
•
At least 15 different antigens are present.
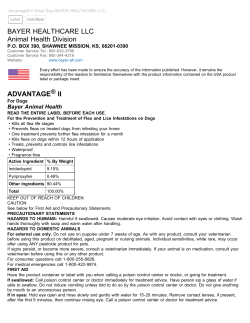
Treatments
Glucocorticoids, antihistamines, essential fatty acids (EFAs), antibiotics, antifungal, anti-flea medication (topical-lotion, gels,
powders, foams, collars, leave-on and oral-nitenpyram, lufenuron), environmental (target all stages)
Ideal Treatment: Safe, non-toxic, non-irritant, Immediate effect (quick knockdown time), Long duration of action, Active against
multiple stages of the flea cycle
Some examples
•
Topical Adulticides: pyrethrums (<0.2% for cats and much higher for dogs- e.g., cyphenothrin in ParastarPlus®),
fipronil (Parastar®, Frontline Plus®), imidicloprid +/- moxidectin (Advantage® and Advantage-Multi®), selamectin
(Revolution®), metaflumizone (Promeris®)-unavailable, dinotefuran (Vectra/Vectra3D®), indoxicarb (Activyl®);
•
Collar: imidicloprid + flumethrin (Seresto®)
•
Oral Adulticide: nitenpyram (Capstar®), afoxolaner (Nexgard®), and spinosad (Comfortis®)
•
Insect Growth Regulators: methoprene (Frontline Plus®, pyriproxifen (Advantage II® and K9Advantix II®;
Vectra/Vectra3D®), lufenuron (Program®Sentinel®/Sentinel Spectrum®)
•
Environment- Pump Sprays; Foggers; Powders; Biologic Agents; Vacuum; Clean Bedding; sodium borate, beneficial
nematodes
Summary of selected insecticides
Insecticide
Chlorpyrifos (Dursban®)
Carbaryl (Sevin®)
Pyrethrin (natural)
Pyrethroids (synthetic)
e.g., cyphenothrin
(Frontline Tritak®; Parastar Plus®)
Chemical Group
Organophosphate
Carbamate
Pyrethrum
Pyrethrum
+/- action on GABA receptors
Fipronil (Frontline®; Parastar®)
Phenylpyrazole
Imidicloprid
(Advantage®/Seresto®/AdvantageMulti®)
Nitenpyram (Capstar®)
Chloronicotinyl (Nicotine)
nitroguanidine
Selamectin (Revolution®)
Spinosad (Comfortis) and
Spintoram (Assurity®; Cheristin®)
Mode of Action
Cholinesterase inhibition (irreversible)
Cholinesterase inhibition (reversible)
Enzyme inhibition, including cytochrome oxidase
Action on voltage-gated sodium channels
Chloronicotinyl (Nicotine)
nitroguanidine
Avermectin
Spinosad
(initial excitement, then paralysis)
Noncompetitive inhibition of gamma amino butyric acid
(GABA)
Bind to post-synaptic nicotinyl receptors
Bind to post-synaptic nicotinyl receptors
Open specific glutamate chloride channels in postsynaptic membranes (GABA, glutamate gated)
Primarily nicotinic acetylcholine receptor; Also GABA
receptors
Spintoram
Indoxacarb (Activyl®)
Oxadiazine
Action on voltage-gated sodium channels
Pyriproxifen (KnockOut®,
Advantage II®))
Lufenuron (Program®;
Sentinel®/Sentinel Spectrum®)
Insect growth regulator (IGR)
Juvenile growth hormone analogue (mimics)
Insect growth regulator
(IGR)/Insect Development
Inhibitor (IDI);
Benzoylphenylurea
Insect growth regulator (IGR)
Terpenoid compound
Inhibit chitin synthesis
Isoxazoline
Inhibition of gamma amino butyric acid (GABA)
Methoprene (FrontlinePlus®)
Afoxolaner
Nexgard®
Juvenile growth hormone analogue (mimics)
© Copyright 2026