Volunteer Reference Manual 2014 - 2015
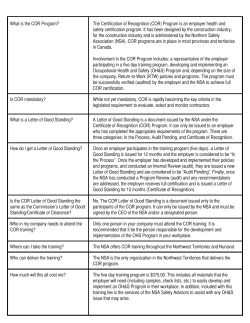
Volunteer Reference Manual 2014 - 2015 Copyright Campus Observation Room Queen’s University, 2014 Updated August 25, 2014 Table of Contents Goals ………………………………………………………………………………………………………………………………………………………… 3 Organization …………………………………………………………………………………………………………………………………..……..... 3 COR Operation 2014 – 15 …………………………………………………………………………………………………………….…………. 3 Staffing …………………………………………………………………………………….………………………………………………………………. 4 Confidentiality ……………………………………………………………………………………………………………………………………….. 4 Harm Reduction Philosophy …………………………………………………………………………………………………………………… 4 Access to COR ………………………………………………………………………………………………………………………….…………...... 5 Volunteer Responsibilities …………………………………………………………………………………………………….…………………. 5 Volunteer Transportation .……………………………………………………………………………………………………….……………… 6 Admission Criteria …………………………………………………………………………………………………………………………………… 6 Transportation of Intoxicated Students ....................................................................................................... 7 Assessment of an Intoxicated Client …………………………………………………………………………………………………....... 7 Admission Assessment Form ....................................................................................................................... 9 Monitoring COR Clients ………………………………………………………………………………………………………………………….. 11 Discharge ……………………………………………………………………………………………………………………………………………….. 11 Record Keeping ……………………………………………………………………………………………………………………………………... 11 COR Observation Checklist …………………………………………………………………………………………………………………….. 12 COR Phone Assessment Protocol................................................................................................................. 13 Shift Duties …………………………………………………………………………………………………………………………………………….. 14 Fire Alarm Policy ……………………………………………………………………………………………………………………………………. 15 First Aid ………………………………………………………………………………………………………………………………………………….. 15 Recovery or Semi-Prone Position ...……….. 15 Airway …………………………………………………. 16 Breathing ………………………………………………. 16 Circulation …………………………………………….. 16 Minor Wounds ………………………………..……. 16 Hyperventilation ………………………………..... 16 Head Injury …………………………………..…….... 16 Emergency Situations ……………………………. 16 Differences ………………………………..……….…. 16 Unconsciousness ………………………..…………. 16 Choking .................................................... 17 Important Phone Numbers ………………………………..…………………………………………………………………………………… 17 General Tips for Dealing with Intoxicated People ………………………………………………………………………………....... 18 Alcohol ……………………………………………………………………………………………………………………………………………………. 19 Absorption ................................................. 19 Metabolism ............................................... 19 Blood Alcohol Content (BAC) .................... 19 Blood Alcohol Level and Effects on Behaviour ….………………………………………………………………………………….... 20 Blood Alcohol Level and Feeling of Intoxication .......................................................................................... 21 Standard Drinks .............................................................................................................................................. 21 Alcohol Poisoning …………………………………………………………………………………………………………………………………… 22 Low Risk Drinking Guidelines …………………………………………………………………………………………………………………… 23 2 GOALS The Campus Observation Room (COR) is an integral part of the Queen’s University initiative to reduce the negative outcomes associated with excessive alcohol use. The Campus Observation Room has two main goals: To reduce the risk of alcohol related injury or death through observation of intoxicated individuals using established protocols. To train a group of Queen's University student volunteers to assess and monitor intoxicated individuals and to provide credible information about safe alcohol use. ORGANIZATION The Campus Observation Room (COR) is affiliated with the Hotel Dieu Hospital Detoxification Centre (Detox), a non-medical detoxification unit providing service to residents of the greater Kingston area. COR activities are funded through Health, Counselling and Disability Services (HCDS), residences and a student interest fee of 65 cents per year per student. In 2011, the students’ funding was renewed for another three years by the AMS and the SGPS. Space, telephone and housekeeping services are provided by the Residences. Overall responsibility for the program rests with Kate Humphrys, the Coordinator of Health Education and Health Promotion Programs at Health, Counselling, and Disability Services. COR OPERATIONS 2014 - 15 Location: COR is located in the basement of Victoria Hall, Rm. A010, behind the Lazy Scholar. Phone: * 613-533-6911 * From Queen’s internal phones - 36911 Dates and Times: Orientation Week: Mon. Sept 1 – Sat. Sept 6 inclusive 8pm – 7am September: Fri. Sept 12 & Sat. Sept 13 Fri. Sept 19 & Sat. Sept 20 Fri. Sept 26 & Sat. Sept 27 8pm – 7am 8pm – 7am 8pm – 7am October: Thanksgiving weekend (Oct. 10, 12) Fri. & Sat. nights, Oct. 3 – Oct. 25 Homecoming Sat. Oct 4 Closed 9pm – 7am NOON – 7am November: Fri. & Sat. nights, Nov 7 – Nov 29 10pm – 7am January: Fri. Jan 9 & Sat. Jan 10 10pm – 7am St. Patrick’s Day: Sat. Mar 14 Tuesday Mar 17 10pm – 7am TBD 3 STAFFING Each year, experienced detoxification workers from the Hotel Dieu Detox Centre are hired to oversee the operation of the COR and the training of volunteer staff. In 2014-15 the staff from Hotel Dieu Detox who will be working in COR will include: Kim Wills, Jessica Stewart, Jacqueline Norris, Lee Hennigar, Marie Champagne, and Catherine Karremans. COR is always supervised by a Detox staff member who ensures that COR is operated in accordance with established procedures and practices. The Detox Supervisor is assisted by trained student volunteers. Student shifts vary in length and it is the responsibility of the Student Volunteer Coordinator to ensure that students are scheduled for each shift. Volunteers also help to promote the benefits of using COR during Orientation Week and throughout the semester. CONFIDENTIALITY Students admitted to the Campus Observation Room are assured that no one is notified of their stay unless they request it information collected is only used to ensure their safety while at COR information about their stay does not become part of their patient record at Health Services (HCDS) or part of their academic or residence file no one working at COR will tell stories about what went on at COR No identifying information may be shared about any student seen in COR. Volunteers are required to sign a Volunteer Confidentiality Agreement prior to their first shift. Any breach of confidentiality will result in the dismissal of the staff person or volunteer. *** This is also applicable to the media. Occasionally, external sources like the Queen’s Journal may ask for you for a comment, as a volunteer, on behalf of the COR. While we are always happy to be involved in ways of increasing awareness of our service, due to its nature, we need to be cautious of what is said to the media. Please do not speak on behalf of the COR without first speaking with Kate. She can be contacted by email at [email protected] or by phone at 613-533-6712. HARM REDUCTION PHILOSOPHY The goal of COR is to ensure students’ safety and, in that spirit, staff and volunteers take a nonjudgmental approach and do not preach the virtues of low risk drinking or abstinence to those who need observation. They may express concern for the potential health or safety risks associated with excessive alcohol use if the opportunity arises. ACCESS TO COR COR is available for all Queen’s students and visitors of Queen’s. Anyone (eg. student, Don, Stu 4 Con, Campus Security, hospital emergency staff, Kingston Police) can call COR and ask for assistance. Access to COR for students living outside Victoria Hall is via the main door of Victoria Hall. COR signs by the front door will display the COR phone number – 36911 - which can be dialled from the outside phone. Alternatively, the desk clerk will answer the doorbell and call COR. If possible, a COR volunteer will come to the front door, but if COR is busy, the visitors will be directed to make their way to COR through the Victoria Hall lobby. Students living in Victoria Hall are encouraged to call COR and let COR staff know they are coming. When possible, the COR staff person may meet them at the front desk, or at the elevator in the Vic Hall basement. **Please note that you need a key in order to operate the elevator** COR VOLUNTEER RESPONSIBILITIES The greatest risk to an intoxicated individual’s safety and well-being is that s/he may vomit and choke. As a COR volunteer, you can prevent a tragic event by monitoring an intoxicated student and getting additional medical support if the situation warrants it. By accepting the role of a COR volunteer, you agree to: Be on time for your assigned shifts. If you are the on-call volunteer, telephone the COR when it opens to let them know how to reach you should you be needed. Arrive early if you are opening COR for the night and assist in set-up. Similarly, if you are closing COR, assist in clean up, including stripping and wiping down the beds and emptying the garbages. Inform the Student Volunteer Coordinator with as much notice as possible if you are unable to meet your shift obligations and assist in finding a replacement volunteer. Wear your COR t-shirt and I.D. badge for each shift. I.D. badges are kept at the Vic Hall front desk so you can pick them up and drop them off at the beginning and end of your shift. Remain sober for all shifts (this includes on-call shifts). Follow the policies and procedures discussed in training and in the manual. Be conscientious in observing the students in your care. Seek advice and take action if a student’s condition worsens or causes you concern for any reason. Err on the side of caution. Assist with COR promotions and education during Orientation Week and throughout the academic year. 5 VOLUNTEER TRANSPORTATION: SAFETY FIRST Shifts may begin or end in the middle of the night. Taxi chits, which entitle you to a free taxi ride between COR and home, are available for volunteers and charged back to the COR budget. We encourage you to use them especially when you have late night shifts. You can pick up a taxi chit at COR. When you use a taxi chit, record the date, your name and your destination on the chit and on the sign-out sheet. Other options for safe transportation home include the AMS walk-home service, or paying for the cab, getting a receipt, and submitting it to the COR supervisor for reimbursement. ADMISSION CRITERIA Intoxicated students are admitted to the COR only if they meet the criteria for admission. This is because COR is strictly an observation unit and does not have the equipment or expertise to deal with situations where there may be trauma, multiple drug use, or a sufficient level of alcohol consumption to cause unconsciousness. The Detox Supervisor ultimately decides whether or not a student seeking admission to COR meets the criteria. If s/he does not meet admission criteria, COR staff must refer the student to an appropriate alternate source of care (HDH Detox Unit, KGH emergency room, etc). Eligibility Criteria Presents with alcohol intoxication only Ambulatory – able to walk alone or with support (may require considerable support) Responsive – must be able to respond, even with a mutter, when you try to rouse them Voluntary – must agree to come to COR Exclusion Criteria 6 Presence of concurrent medical illness Presence of concurrent trauma Concurrent use of other substances (see Appendix A for more information) Non-ambulatory and/or non-responsive (passed out and/or unable to rouse) Unwilling to come into or stay at COR Presence of obvious psychiatric disturbance Violent or aggressive behaviour Presence of significant withdrawal states: o Auditory of visual hallucinations o Seizures o Acute agitation TRANSPORTATION OF INTOXICATED STUDENTS Usually students are expected to get to COR at their own expense, however, COR will cover the cost to transport students in taxis in two instances. 1. Students may be discharged directly from the KGH Emergency Dept. to COR. Emerg will call COR to notify the staff that a student is coming and then they will send the student in an Amey’s Taxi. A COR volunteer will meet the taxi at the front of Victoria Hall with a taxi chit. 2. Students from Waldron Tower, West Campus or off-campus student housing, can be transported to COR via Amey’s Taxi, at COR’s expense. A friend will need to accompany the intoxicated student in the taxi, bring him or her into COR, and pick up a taxi chit to cover the cost of the taxi. Come morning, students may also be sent back to West Campus and Waldron Tower in a taxi. ASSESSMENT OF AN INTOXICATED CLIENT At the Door: One or two volunteers/staff members go to the door to deal with an intoxicated client. As you approach the door observe the following: Signs and level of intoxication: e.g. slurred speech, staggering gait Any visible signs of injury (see the section on first aid for more details) Any sign that the client is concealing liquor bottles, medication containers, etc. Evidence of agitation, aggression, or reluctance to be there First Contact with the Client: Introduce yourself Ask for their name Speak clearly and calmly Explain what will happen Ask permission before you make any physical contact with them For example “Hi, my name is Jack. What’s yours?” (Assume the person needing help is John) “Hi John. I just need to ask you a couple of quick questions and then you can lie down for a while. Is that okay with you? Would you like to sit down for a minute? Can I help you here?” COR staff should attempt to calm the aggressive client by talking with them in a non-threatening manner. If attempts to calm the aggressive client fail, they will be advised to go elsewhere, and COR staff should call campus security. 7 Important Notes: Once students who are at risk of hurting themselves or others (whether intentionally or not) come to your attention, you are responsible to ensure they are not left in a position where they will cause harm to themselves or to others. Fortunately, Queen’s has resources to help in these situations: * Clients who are non-ambulatory (non-responsive) or showing signs of injury will not be admitted to the COR. Instead, they will be sent to the KGH Emergency. Call the Queen’s Emergency Reporting Centre (ERT) at 36111. Specify the problem and request help from Queen’s First Aid (QFA) or an ambulance. * Clients who are aggressive and/or uncooperative at the door will not be admitted to COR. If they are not safe to be left on their own, call 36111 for help. The ERT will dispatch Campus Security or the Kingston Police. When COR staff determine that the person at the door meets the admission requirements, they then escort the person into COR, offering assistance to walk safely when needed. When two or more clients arrive for admission at the same time, follow the same procedure for each client. Request that others who accompany the client wait. If possible have a COR staff person stay with those waiting at the door. Once Inside COR: 8 Help the client to a chair Put a bucket beside the chair If the client needs to use the washroom, escort them Look for a medic alert tag (bracelet, necklace) Complete the COR Assessment Report (see pages 9 - 10) Once you have all the necessary information, assist the client to a bed and lay them in the recovery position COR Admission Assessment Date _____/ _____/______ Male / Female Time: __________________ Res / Off-campus / Visitor to Queen’s Name _________________________ Keys? Yes Address/Residence ________________________ If no, plan for the morning? __________ No Contact Person’s Info and Phone #: ____________________________________________________ ************************************************************************************************* General Observations: Circle the appropriate descriptor. Level of intoxication High Moderate Level of consciousness Responds to verbal cues: Orientation: Mild With answers Knows name With groans/mutters response Knows location No Knows day/month/year Reported consumption (what, how much) ________________________________________ ___________________________________________________________________________ Precipitating factors _________________________________________________________ (Event, situation, etc.)_________________________________________________________ Respiration Normal Shallow Labored Skin (Color) Normal Pale Flushed (Touch) Warm/dry Cold/clammy Warm/moist Cold/dry Unsteady Staggering Gait Vomiting Yes, Before COR Blue/Purple Requires assistance Yes, at Present No Comments _______________________________________________________________ ___________________________________________________________________________ 9 Medic Alert Yes No Comments: _________________________________________________________________ _____________________________________________________________________________ Allergies Yes No Comments: _________________________________________________________________ _____________________________________________________________________________ History of recent fall, Recent Head/Body Injuries Yes No Comments: _________________________________________________________________ _____________________________________________________________________________ Medical Conditions / Medications Yes No Comments: _________________________________________________________________ _____________________________________________________________________________ Eligible for service Yes No Observation / follow-up notes ___________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ Assessed by (please print name): _______________________________ Volunteer’s/Staff signature_________________________________ ************************************************************************ Discharge Date: ______/_____/______ Time: _______________________ Discharge Note (condition of client, discharge time, discharged to where & with whom) ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________________________________ Staff/Volunteer’s signature 10 ________________________________________________ MONITORING COR CLIENTS Clients must be monitored at all times. Volunteers watch for changes in cognition, colour, breathing and consciousness. Complete the Observation Checklist (page 12) every 15 – 30 minutes as the person’s condition warrants. Encourage the client to sleep. If they wish to talk, allow them to speak and be supportive. Disruptive clients will be asked to behave and if they won't comply, they will be discharged. Call Campus Security for assistance. If you believe a disruptive client might be a danger to themselves or others, you must notify the Queen’s Emergency Response Team (ERT) at 36111 about their discharge from COR and together, make alternate arrangements. DISCHARGE Clients should be encouraged to stay until they are no longer intoxicated. In the event that a client who wants to leave is still intoxicated and, in the judgement of the COR staff, a danger to themselves, the COR staff will: Try to persuade them to stay Arrange for a responsible friend, roommate or Don to look after them Call 36111. ERT will dispatch Campus Security or the Kingston Police When a client is able to leave: Record the date and time of discharge on the admission form Complete the info on the client’s condition and how/with whom they left Sign the bottom of the form A client who is still intoxicated when the COR is closing may be transferred to the HDH Detox Centre or picked up by a responsible, sober friend. The friend should be taught how to monitor the intoxicated individual, and made aware of the risks and resources for getting help. RECORD KEEPING The client records and logbook entries are the legal records of the activities at COR. It is important that all documentation be completed and signed. The Detox Supervisor will ensure that an accurate record of each client’s admission to and discharge from COR is kept. A nightly log is also kept detailing the name(s) of the Detox Supervisor, student volunteers on duty, and telephone inquiries. Clients’ admissions and discharges are also documented (including the time, condition of the individual, his/her willingness to stay, information on accompanying individuals). The logbook also includes a description of anything noteworthy that happens at COR (fire alarms, difficult or unexpected behaviour/situations and the actions taken). These records are secured at the end of each shift and reviewed by the Health Promotion Coordinator at the end of each weekend. They are held in a confidential spot separate from all other patient/client/resident/ student files. 11 COR Observation Checklist To be completed every 15 – 30 minutes. Name: ________________________________ Date: __________________________________ Bed number: _______________ Time Awake Asleep Ambulatory Respiration Normal Labored or shallow breathing Skin Normal Clammy Flushed Blue/purple Warm/dry Coherent Requires rousing Vomiting Requires assistance Taking fluids Volunteer Initials Volunteer Name(s) _______________________________________________________________ 12 COR Phone Assessment Protocol Date _____/ _____/______ Time: ________________________________ Name: ___________________________ Phone Number: ______________________ Location: ________________________ ************************************************************************ Reported Consumption (what, how much, time span, when): __________________________________________________________________________ __________________________________________________________________________ Level of consciousness Awake Asleep (can rouse) Cannot rouse Response to verbal cues With answers With groans/mutters No response Staggering Requires assistance No self weight-bearing No Yes Gait Head injury? Other medical conditions? No Yes Any other substance use? No Yes AT THIS POINT, IF FURTHER MEDICAL ATTENTION IS NOT OBVIOUSLY REQUIRED, ALLOW THE DETOX STAFF ON DUTY TO DECIDE BETWEEN ADVISING THE STUDENT TO COME IN TO COR OR TO BE MONITORED AT HOME BY A RESPONSIBLE, SOBER FRIEND. REMEMBER THAT ONCE STUDENTS WHO ARE AT RISK OF HURTING THEMSELVES OR OTHERS COME TO YOUR ATTENTION, YOU ARE RESPONSIBLE TO ENSURE THAT THEY ARE NOT LEFT IN AN UNSAFE SITUATION. Assessed by: ___________________________________________ Volunteer’s/Staff Signature: __________________________ IF ANY RIGHT COLUMN RESPONSES, IMMEDIATELY CALL THE ERT AT 36111 OR CALL 911 13 SHIFT DUTIES Opening / Closing All COR volunteers must pick up their ID badge at the Vic Hall front desk when they arrive for a shift and drop it off when they leave. The first person to arrive signs out the COR keys and any COR supplies left at the front desk. At the start of the night, volunteers help make up the beds, put new bags in all the garbage cans, etc. In the morning, volunteers help strip the linens, empty the garbage cans, and wipe down all the bed surfaces. When closing up, seal all client notes & log pages in an envelope, and drop off the envelope and key at the Vic Hall front desk. Ensure that the envelope goes on the COR shelf and is not put through Queen’s mail. The envelope should be labelled clearly with the words COR, CONFIDENTIAL and HOLD (on COR shelf) FOR PICK UP BY KATE HUMPHRYS. Log Book There is a daily log book in which the following is to be recorded on each shift: COR staff and volunteers on duty; times when they arrive and when they leave All admissions and discharges. These should be recorded in red ink. Information on each client includes the time of admission and discharge All phone calls and visitors Any other pertinent information or unusual occurrences, eg. difficult or unexpected behaviour, fire alarms, calls to Campus Security or Queen’s First Aid, unusual situations and the actions taken, etc. The completed client information forms and logs are never left at COR at the end of a shift. Make sure they are placed in a sealed envelope that should be left at the Vic Hall Front Desk. The Detox Supervisor will notify the KGH Emergency Department that COR is open. Volunteers will check at the beginning of each shift that directional signs are up at the front door and throughout Vic Hall and replace as necessary. Notes on Cleaning Up Rubber gloves are always worn when performing any cleaning duty or assisting students. The Detox Supervisor will ensure that all cleaning is done in accordance with WHMIS standards. Dirty linen and garbage should be placed outside the COR at the end of each shift. If the floor needs cleaning, a note should be posted on the door for the Residence Housekeeping staff. Any spills or accidents on the carpet should be reported right away to the after-hours housekeeping staff. Notify the Vic Hall after-hours housekeeping staff at 613-561-2665 or the Health Promotion Coordinator at x36712 if additional supplies are needed. You can leave a message for Kate at any time of the night and she will get it on Monday morning. 14 FIRE ALARM POLICY Upon hearing an alarm: The Detox Supervisor appoints one of the COR Volunteers to go to the Vic Hall Front Desk and talk with the Security Supervisor or the Fire Chief. Tell them how many people are in the COR room. Know the general condition of the COR clients so you can estimate how much help is needed to evacuate them. They will check on the location of the alarm. If the fire is not in the vicinity of COR, everyone will be allowed to stay in COR throughout the alarm. If the fire is near the COR area, they will ask you to evacuate. Ask for assistance with the evacuation if necessary. The designated assembly area for Victoria Hall is across Bader Lane. In case of bad weather, COR clients should be moved to Gordon/Brockington Hall. When the “all clear” signal to re-enter is given by either the Fire Department or Campus Security, assist the clients’ re-entry to the building. Note: All volunteers should know the locations of the nearest exits to COR. FIRST AID The Recovery or Semi-Prone Position This is a position where the victim is laying on their side with their head resting on their bottom arm: 1. Raise the person's closest arm above his or her head. Prepare to roll him/her towards you. 2. Gently roll as a unit. Guard his/her head as you roll him/her. Bend the top hip and knee to 90 degrees. 3. Tilt head back slightly to maintain airway and position the face and mouth downwards to allow fluids to drain out of the mouth. Tuck nearest hand under cheek to help maintain head tilt. 15 Airway Watch out for vomit blocking an airway. Turn the client into the semi-prone position and clear out any obstructions with your finger if necessary. Never go beyond where you can see when scooping out vomit. Breathing Alcohol is a depressant that slows down the body's systems. Breathing rates below 10 per minute and over 30 per minute are considered dangerous and further medical attention should be sought. Circulation The pulse should also be monitored. If a dramatic drop or a continual decrease over an appreciable time period is noted, then medical help is needed. Minor Wounds A person with a bleeding wound that cannot be stopped by direct pressure needs to go to the hospital. As well, any cut over 2 cm long or 1 cm deep requires stitches. Wounds from animals tend to be jagged (ripped) and dirty and therefore require professional medical attention (i.e. stitches, vaccines). Any wound is treated the same way. Use the acronym R.E.D. to remember: REST, ELEVATION, and DIRECT PRESSURE. sit/calm the patient down elevate the wound above the heart cover the wound with a clean material (i.e. gauze) apply pressure over the wound. Remember to wear disposable gloves. Hyperventilation Do NOT put a bag over their mouth!! Just try to calm them down. Remember it is dangerous to have a breathing rate over 30 breaths per minute. Head Injuries People with head injuries may behave as if they are drunk. If a person has a large bump or cut on their head or if there is a history of a fall prior to coming to COR, consider a head injury as a possible reason for their behaviour. It is better to err on the side of caution and have the individual checked out by QFA (Queen’s First Aid) or a physician at the KGH Emergency Dept. EMERGENCY SITUATIONS The following situations require prompt action. Call 36111 and request QFA or an ambulance. Differences Any differences between one side of the body and the other are considered to be serious. Differences in the capillary refill, pupil size or reactivity, response to pain stimuli or strength, point to an underlying problem that may require hospitalisation. Call 36111 and ask for help. Unconsciousness Anyone who is unconscious to the degree where they cannot be aroused by pain is in a dangerous 16 condition and must go to the hospital. Immediately call 36111 and ask for help. Choking Please refer to your CPR certifying agency’s manual for current choking procedures. If you come across an unconscious person in or out of the COR you should all for immediate assistance. 36111 (on-campus) or 911 (off-campus). Request an ambulance. IMPORTANT PHONE NUMBERS COR 36911 (Queen’s internal) 613-533-6911 (external) ERT 36111 613-533-6111 Emergency Response Team * Call for any emergency – medical, safety, access, etc. * Specify problem and what is needed, eg. ambulance * ERT is able to dispatch Campus Security, Queen’s First Aid, ambulance, or Kingston Police Hotel Dieu Detox 613-549-6461 24 / 7 advice about detox, alcohol symptoms KGH Emergency 613-548-2333 Kingston Police 613-549-4660 Amey’s Taxi 613-546-1111 Housekeeping 613-561-2665 After-Hours Housekeeping, Vic Hall * For quick delivery of extra supplies, eg. sheets, blankets, towels, cleaning solution, rubber gloves, fans, cots, etc. 613-533-6712 36712 (internal) Leave a message about any issues that need follow-up, questions, requests for more / different snacks COR Coordinator Kate Humphrys Victoria Hall Front Desk x32531 Helpful for many things! 17 GENERAL TIPS for DEALING with INTOXICATED PEOPLE C.A.B.B.Y: C: Stay calm: take a deep breath and don't transfer your anxiety to the individual in trouble. A: Assess the situation: is the person conscious or passed out, are they breathing, how much has the person had to drink, is he/she talking sense, are they mobile? B: Be aware of the main dangers: Choking: either on their own vomit or on food, drink or medication. Injury: because co-ordination, balance and judgment are affected by alcohol, a person may fall or take risks they would not take if they were sober. Unconsciousness or respiratory problems: as the blood alcohol level rises, the basic functions of heart rate and breathing are affected, which could result in respiratory or cardiac arrest. See the information on emergency first aid. B: Work with a buddy. Y: You are an important resource. Remember to look out for your own safety too. DOs and DONTs DO Keep your distance. Explain what you intend to do before approaching or touching the person. Speak in a clear, firm, calm and reassuring manner. Stay with a person who is vomiting. Position them in the recovery position. Watch the person's breathing. Call for help if there are changes in the rate or sound of the breathing. Keep the person calm and comfortable. DON'T 18 Laugh at, get in the face of, express anger towards, or argue with someone who has been drinking. Attempt to physically restrain an intoxicated person. It usually makes a touchy situation worse. Give food, liquids or drugs to sober someone up. Only time can do that. COR PROMOTIONS/EDUCATION INFORMATION As a student volunteer, you are expected to participate in a variety of different promotional and educational activities throughout the year. The focus of these activities is a more proactive approach with students – educating about the alcohol consumption and promoting safe consumption strategies, and of course, promoting the services and hours of the COR. These activities happen at various times throughout the year, some examples include: 1) Orientation Week – COR volunteers host activities/presentations with faculty orientation weeks. Activities can range from interactive sessions with beer goggles to short talks about the foundational principles of COR and promotion of services. 2) Monthly Promotions Activities – each student volunteer is expected to sign up for a monthly promotions outreach. These can include social media updating, poster development and distribution, and creation of promotional materials, among other things. This will be explained further in training. 3) Residence Walkabouts – COR volunteers go into residences with Residence Dons and engage first year students with interactive activities designed to educate about an alcohol related topic – alcohol poisoning, standard drink sizes, etc. We also distribute branded COR material (often as prizes) to help students remember us! Please give away all the materials you are provided with as possible, we purchase it to distribute it to students, not to keep it in a box in the office! Key Messages for Outreach During Outreach Activities COR volunteers should focus on promoting the following key messages: I. COR Services. Our primary objective for most outreach is to spread the word about COR, sharing basic information such as what is COR, where we are located, when we are open, what we do, and how to use / contact COR, etc. COR is a service for all Queen’s students & their guests – everyone can use COR or call for advice. II. COR Philosophy. Our goal is to ensure student safety, using a harm reduction philosophy. COR is non-judgmental, confidential and voluntary. III. Alcohol Harm Reduction. Some outreach includes alcohol safety / harm reduction messages. This is an opportunity to help students learn more about being safe & smart about alcohol. We don’t preach abstinence, but we also do not encourage unsafe drinking. We understand and respect that everyone has their own opinions about alcohol – some students do not drink, others do. We want everyone to be safe and smart about drinking – and that includes using COR services if needed. Some messages we promote include: standard drink sizes, alcohol poisoning & the recovery position, eating before you drink, etc. COR is a very well-respected service on campus. We are known for our student-centred, realistic and ‘fun’ approach. This is a reputation that we value and strive to maintain during outreach. 19 GENERAL INFORMATION ABOUT ALCOHOL Alcoholic beverages are drinks that contain ethanol, a colourless liquid with a strong, characteristic odour. Ethanol, or alcohol as it is commonly known, is a psychoactive drug that has a depressant effect on the central nervous system. Short-term effects of drinking alcohol include intoxication, dehydration and in high concentrations, alcohol poisoning. Alcohol is the most commonly used recreational drug in the world. It is produced and consumed in most parts of the world and is an important component of many social events in many cultures. Absorption The alcohol in drinks is absorbed directly into the bloodstream within 1 – 2 hours of consumption. Up to 20% of alcohol can be absorbed from the stomach. The rest enters the bloodstream through the small intestine. Absorption is slowed by having food in the stomach and diluting the alcohol (adding mix to spirits for example), and is speeded up by the presence of carbonated beverages, by greater alcohol concentrations, and by stress. Once in the bloodstream, alcohol, which is water soluble, reaches all the body’s organs and cells in minutes. Metabolism As it circulates in the bloodstream, alcohol is metabolized at a fixed rate. On average, it takes approximately 1½ - 2 hours to metabolize one standard drink. 95% of alcohol is metabolized in the liver while the other 5% is excreted directly through respiration, perspiration and urination. Metabolism of alcohol depends on the quantity of enzymes in the liver and cannot be sped up by exercising, drinking coffee or sweating. Males have more of these enzymes than women, and consequently, tend to metabolize alcohol more quickly. The body acts like a funnel when it’s processing alcohol. No matter how much we drink, our bodies get rid of alcohol at a fixed rate. We can drink alcohol much faster than we can expel it from our bodies. For example, if someone drinks 6 standard drinks in an evening, their body will not be free of all alcohol until approx. 9 - 12 hours after they start absorbing their first drink. Blood Alcohol Content (BAC) BAC, or blood alcohol level (BAL) is the quantity of alcohol in the bloodstream. It is often written as a percentage that represents milligrams (mg) of alcohol per 100 millilitres (ml) of blood. How fast BAC rises and how intoxicated one gets depends on many factors that can be categorized into two main groups. 1. How You Drink 20 Quantity: The more alcohol consumed in a period of time, the higher the BAC rises. This factor most affects the BAC. Speed: The faster alcohol is consumed, the faster the BAC rises. Food: Food in the stomach slows (but does not prevent) the absorption of alcohol and delays the rise in BAC. 2. The Proportion of Water in the Body Sex: If a man and a woman of the same weight drink the same amount of alcohol, the woman’s BAC will usually be higher. This is because women have a higher % of body fat and lower % of body water than men. Weight: A lighter person will have a higher BAC than a heavier one because smaller people’s bodies contain less water so the same amount of alcohol is more concentrated. Age: Older people have a lower percentage of water in their bodies than younger people and will have a higher BAC than a young person who has consumed the same amount of alcohol. (BAC) & EFFECTS ON BEHAVIOUR BAC 0.05% 0.08% 0.12% 0.14% 0.15% Average # of Drinks 1 - 2 drinks 3 - 4 drinks 4 - 6 drinks Behaviour * * * * usually a feeling of well-being judgment and the ability to self-monitor slightly affected co-ordination & level of alertness lowered increased risk of an accident while driving * * * * reaction times significantly slowed muscle control and speech impaired reduced night & side vision judgment and self-monitoring abilities increasingly affected * * consistent and major impairment of mental and physical control slurred speech, blurred vision, markedly increased reaction times loss of motor control; needs help to move about mental confusion double vision 0.20% 6 - 9 drinks * * * 0.25% 7 - 10 drinks * staggering and severe motor disturbances 0.30% 8 - 12 drinks * minimum conscious control of mind and body; not aware of surroundings 0.35% 9 - 13 drinks * "passed out", surgical anaesthesia; lethal dosage for a small % of individuals 0.40% 0.60% 11 - 20 drinks * * severe circulatory and respiratory depression, deep coma. lethal dose for 50 % of individuals Remember, this is only an estimation based on average metabolic rate. Every person reacts differently to alcohol. 21 BAC AND FEELING INTOXICATED You cannot judge your BAC or your level of intoxication by how you feel because: * Both BAC and how fast alcohol is being absorbed affect how intoxicated someone feels. The more alcohol in a drink, the more quickly it is absorbed and the more intoxicated someone feels. Drinking several diluted drinks leads to feeling less intoxicated than indicated by the BAC because the alcohol is being absorbed at a slower rate. * People feel more intoxicated when their BAC is rising than when it is falling. For example, in the morning after heavy drinking, people feel they are sober even though their BAC may still be very high. For example, a 150 lb. male who drinks 12 drinks between 8pm and midnight will still have a BAC of almost twice the legal limit at 9am the next morning. * Regular drinkers may develop a tolerance to alcohol. This means their bodies have adapted to alcohol and that they need more alcohol and a higher BAC to feel the same effect. People who have developed tolerance to alcohol may not feel intoxicated and may seem to act normally even though their BAC is above the legal limit. In fact, their fine motor control, attention, judgment and ability to drive are still impaired. Remember, impaired judgment means people don’t have the capacity to accurately judge their abilities. STANDARD DRINKS A standard drink contains 1 serving or 0.6 oz or 17 ml of alcohol. Each of the following is one standard-sized drink: Regular beer Cooler Beer or Cooler Wine Fortified wine Liquor 4 – 5% alcohol 4 – 5 % alcohol 7% alcohol 10 – 12% alcohol 16 – 18% alcohol 40% alcohol 12 oz. 12 oz. 8 oz. 5 oz. 3 oz. 1.5 oz 341 ml 341 ml 230ml 142 ml 85 ml 43 ml How Many Standard Drinks in a Bottle? Hard Liquor (40% alcohol) 13 oz. / 375 ml 26 oz. / 750 ml 40 oz. / 1.14 L 9 standard drinks 18 standard drinks 27 standard drinks Wine (10 – 12% alcohol) 26 oz. / 750 ml 35 oz. / 1 L 5 standard drinks 7 standard drinks Beer / Coolers (5% alcohol) 20 oz. / 1 pint 35 oz. / 1 L 1.7 standard drinks 3 standard drinks 12 oz. / 341 ml 35 oz. / 1 L 1.4 standard drinks 4 standard drinks (7% alcohol) 22 ALCOHOL POISONING Alcohol depresses nerves that control involuntary actions such as breathing and the gag reflex (which prevents choking). A fatal dose of alcohol will eventually stop these functions. It is common to vomit after drinking excessive alcohol since alcohol is an irritant to the stomach. There is then the danger of choking on vomit, which could cause death by asphyxiation in a person who is not conscious because of intoxication. You should also know that a person's BAC can continue to rise even while he or she is passed out. Even after a person stops drinking, alcohol in the stomach and intestine continues to enter the bloodstream and circulate throughout the body. It is dangerous to assume the person will be fine by sleeping it off. Critical Signs for Alcohol Poisoning Mental confusion, stupor, coma, or person cannot be roused Vomiting Seizures Slow breathing (fewer than 10 breaths per minute) Irregular breathing (10 seconds or more between breaths) Hypothermia (low body temperature), bluish skin color, paleness What Should I Do If I Suspect Someone Has Alcohol Poisoning? If there is any suspicion of an alcohol overdose, contact the emergency response team by calling 36111 from an internal campus line Do not wait for all symptoms to be present If not on campus, call 911 for help What Can Happen to Someone With Alcohol Poisoning That Goes Untreated? Victim chokes on his or her own vomit Breathing slows, becomes irregular, or stops Heart beats irregularly or stops Hypothermia (low body temperature) Hypoglycemia (too little blood sugar) leads to seizures Untreated severe dehydration from vomiting can cause seizures, permanent brain damage, or death Even if the victim lives, an alcohol overdose can lead to irreversible brain damage. Rapid binge drinking is especially dangerous because the victim can ingest a fatal dose before passing out. Don't be afraid to seek medical help if someone exhibits the signs of alcohol poisoning. Better to err on the side of caution and be safe. 23 LOW RISK DRINKING GUIDELINES At Queen’s, most students usually drink responsibly with low incidences of negative outcomes. In the 2008 and 2009 and 2012 and 2013 Student Health Surveys, over 60% of students said they consumed 4 or fewer drinks the last time they partied. Low risk drinking guidelines as recommended by the Centre for Addiction and Mental Health are as follows: Reduce your long-term health risks by drinking no more than 10 drinks a week for women, with no more than 2 drinks a day most days. 15 drinks a week for men, with no more than 3 drinks a day most days. Plan non-drinking days every week to avoid developing a habit. Exceptions There are times and circumstances when the safest course of action is to not drink or to drink at levels considerably lower than the guidelines. Do not drink when you are: Driving a vehicle or using machinery and tools Taking medications or other drugs that interact with alcohol (such as sedatives, painkillers or sleeping pills) Doing any kind of dangerous physical activity Living with mental or physical health problems Living with alcohol dependence Pregnant, planning to be pregnant or breastfeeding Doing any kind of dangerous physical activity Responsible for the safety of others Making important decisions Thank you so very much for volunteering your time to help make our campus safe. a safer place for all!! 24 Appendix A: Alcohol and Other Drugs At COR, we only admit students who are intoxicated on alcohol and not on other drugs or substances. Our volunteers do not receive the necessary training in order to understand or know how to handle drug interactions. Here is some information on common recreational drugs used by the Queen’s student population. Remember, if a student has ingested other substances, COR is not the right place for them. Marijuana (weed, pot, reefer, grass, dope, hash) Effects: - mood lift - relaxation - heightened sensory perception - increased appetite - decreased anxiety - blood-shot eyes - tachycardia (racing heartbeat) - dizziness - confusion - paranoia Marijuana and alcohol, when taken together, intensity each other’s effects. Having alcohol in your blood can potentially cause your body to absorb the active ingredient tetrahydrocannabinol (THC) faster. While some users combine these two substances with no problems whatsoever, it can lead to complications and heightened side effects. For example, marijuana's tendency to reduce nausea and suppress the gag reflex can make it difficult for an individual to vomit, thus increasing the risk of someone choking due to alcohol poisoning. On the other hand, it is also possible for a user to get a severe case of "the spins" due to the compounded dizzying effects of both alcohol and marijuana; this often results in severe nausea and vomiting. Cocaine (blow, coke, crack, snow, etc.) Effects: - increased alertness - increased wakefulness - euphoria - decreased fatigue - increased heart rate (tachycardia) - sweating - aggressive or violent behavior - hallucinations and delusions - restlessness/irritability - paranoia Research has found that the human liver combines cocaine and alcohol to produce a third substance, cocaethylene, which increases the depressive effects of alcohol and intensifies cocaine’s euphoric effects. Cocaethylene is associated with a greater risk of sudden death than cocaine alone. It also stays in your system longer than either alcohol or cocaine on its own, and can be fatal for up to 12 hours after it is taken. MDMA (M) Effects: 25 - euphoria - increased empathy - heightened sensory perceptions - mild hallucinations - increased energy - jaw clenching / teeth grinding - overheating - dehydration - muscle spasms - increased heart rate (tachycardia) - post-use depression Mixing MDMA with alcohol increases the risk of nausea and vomiting, and can lead to dangerous dehydration and overheating. The diuretic effects of alcohol, combined with a hot clubbing environment, makes it very difficult to stay hydrated when you drink while on MDMA. The ‘down’ you experience after the ‘high’ is also much more severe when alcohol is in the mix. Study Aids (Prescription Amphetamines) (Ritalin, Adderall, Dexedrine) Effects - increased alertness/concentration - wakefulness - talkativeness - efficiency - mood lift - increased heart rate (tachycardia) - dizziness - paranoia - headache - dry mouth - difficulty sleeping - hallucinations (often from lack of sleep) Amphetamines are widely prescribed to treat Attention Deficit Hyperactivity Disorder (ADHD). Counter intuitively, individuals with ADHD tend to calm down when under the influence of these drugs, and individuals without ADHD become hyperactive. Mixing amphetamines, a stimulant, and alcohol, a depressant, often results in a suppressed effect of both. Therefore, people tend to drink much more than usual, often dangerous levels, without feeling the effects. In addition, drinking alcohol while taking an amphetamine can lead to an increased likelihood of aggressive, violent, or paranoid behaviour. *http://www.dartmouth.edu/~healthed/groups/dapa/otherdrugs/ *http://www.drinkaware.co.uk/facts/alcohol-and-illegal-drugs 26
© Copyright 2026